Abstract
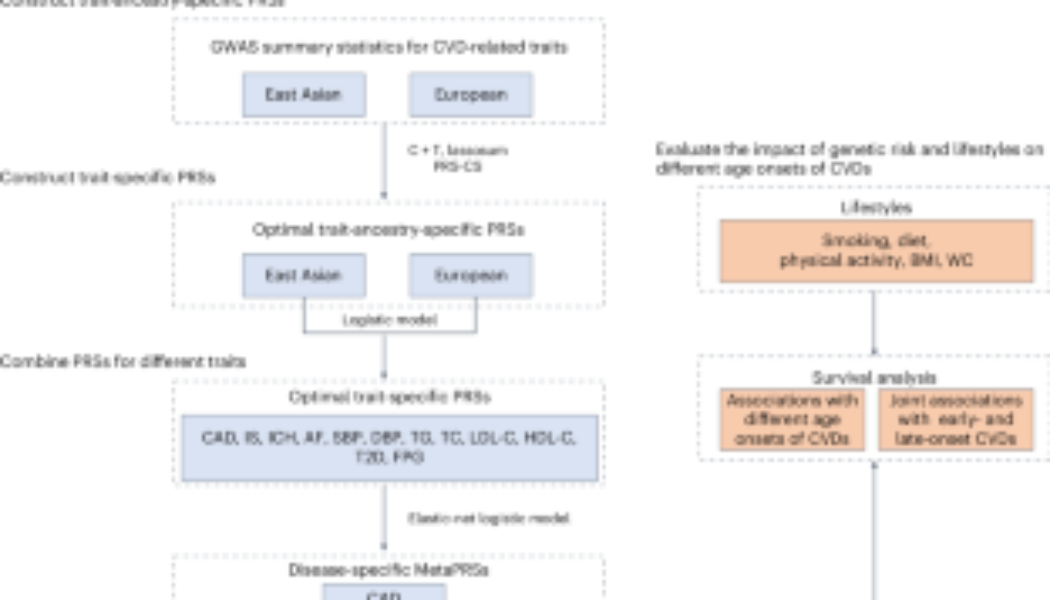
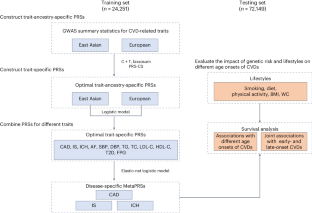
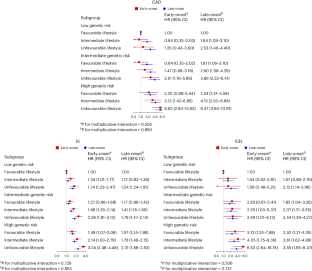
Understanding the interactions between genetic risk and lifestyles on different types and age onsets of cardiovascular disease (CVD) risk can help identify individuals for whom lifestyle changes would be beneficial. Here we developed three polygenic risk scores, called MetaPRSs, for coronary artery disease, ischaemic stroke and intracerebral haemorrhage by combining PRSs for CVD and CVD-related risk factors in 96,400 participants from the prospective China Kadoorie Biobank. Genetic and lifestyle risks were categorized by the disease-specific MetaPRSs and the number of unfavourable lifestyles. High genetic risk and unfavourable lifestyles were found to be more strongly associated with early than late onset of CVD outcomes in men and women. Change from unfavourable to favourable lifestyles resulted in 14.7-, 2.5- and 2.6-fold greater reductions in incidence rates of early-onset coronary artery disease and ischaemic stroke and late-onset coronary artery disease in high than low genetic risk group. Young adults at high genetic risk may have larger benefits in preventing CVD from lifestyle improvements.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Additional access options:

Data availability
CKB data are available to all bona fide researchers. Details of how to access and details of the data release schedule are available from www.ckbiobank.org/site/Data+Access. As stated in the access policy, the CKB study group must maintain the integrity of the database for future use and regulate data access to comply with prior conditions agreed with the Chinese government. Data security is an integral part of CKB study protocols. Data can be released outside the CKB research group only with appropriate security safeguards. Genome-wide association data supporting this study are available from the GWAS catalogue (https://www.ebi.ac.uk/gwas/studies/GCST005195, https://www.ebi.ac.uk/gwas/studies/GCST90104540, https://www.ebi.ac.uk/gwas/studies/GCST90018644, https://www.ebi.ac.uk/gwas/studies/GCST90043994, https://www.ebi.ac.uk/gwas/studies/GCST90018650, https://www.ebi.ac.uk/gwas/studies/GCST006414, https://www.ebi.ac.uk/gwas/studies/GCST004373, https://www.ebi.ac.uk/gwas/studies/GCST006624, https://www.ebi.ac.uk/gwas/studies/GCST90018752, https://www.ebi.ac.uk/gwas/studies/GCST006630, https://www.ebi.ac.uk/gwas/studies/GCST90018732, https://www.ebi.ac.uk/gwas/studies/GCST90239664, https://www.ebi.ac.uk/gwas/studies/GCST90018755, https://www.ebi.ac.uk/gwas/studies/GCST90239676, https://www.ebi.ac.uk/gwas/studies/GCST90018754, https://www.ebi.ac.uk/gwas/studies/GCST90239658, https://www.ebi.ac.uk/gwas/studies/GCST90018741, https://www.ebi.ac.uk/gwas/studies/GCST90239652, https://www.ebi.ac.uk/gwas/studies/GCST90018736, https://www.ebi.ac.uk/gwas/studies/GCST90002232), the NBDC Human Database (https://humandbs.dbcls.jp/en/hum0014-v32) and the DIAGRAM consortium (http://diagram-consortium.org/downloads.html). The 1,000 genome project reference panels are available from https://mathgen.stats.ox.ac.uk/impute/1000GP_Phase3.html.
Code availability
Analysis code for this study is available at https://github.com/pkuepisd/Genetic-risk-lifestyles-and-early-onset-CVD.
References
-
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
-
Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization (IHME, University of Washington, 2020); https://vizhub.healthdata.org/gbd-compare
-
Wang, H. et al. Pathogenesis of premature coronary artery disease: focus on risk factors and genetic variants. Genes Dis. 9, 370–380 (2022).
-
Mosley, J. D. et al. Predictive accuracy of a polygenic risk score compared with a clinical risk score for incident coronary heart disease. JAMA 323, 627–635 (2020).
-
Elliott, J. et al. Predictive accuracy of a polygenic risk score-enhanced prediction model vs a clinical risk score for coronary artery disease. JAMA 323, 636–645 (2020).
-
Khan, S. S. et al. Predictive utility of a validated polygenic risk score for long-term risk of coronary heart disease in young and middle-aged adults. Circulation 146, 587–596 (2022).
-
Marston, N. A. et al. Predictive utility of a coronary artery disease polygenic risk score in primary prevention. JAMA Cardiol. 8, 130–137 (2023).
-
Manikpurage, H. D. et al. Polygenic risk score for coronary artery disease improves the prediction of early-onset myocardial infarction and mortality in men. Circ. Genom. Precis. Med. 14, e003452 (2021).
-
Jukarainen, S. et al. Genetic risk factors have a substantial impact on healthy life years. Nat. Med. 28, 1893–1901 (2022).
-
Yang, S. et al. Associations of polygenic risk scores with risks of stroke and its subtypes in Chinese. Stroke Vasc. Neurol. https://doi.org/10.1136/svn-2023-002428 (2023).
-
Yang, S. et al. Minimal improvement in coronary artery disease risk prediction in Chinese population using polygenic risk scores: evidence from the China Kadoorie Biobank. Chin. Med. J. 136, 2476–2483 (2023).
-
Ma, Q. et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 6, e897–e906 (2021).
-
Lu, X. et al. Development and validation of a polygenic risk score for stroke in the Chinese population. Neurology 97, e619–e628 (2021).
-
Myserlis, E. P. et al. A genomic risk score identifies individuals at high risk for intracerebral hemorrhage. Stroke 54, 973–982 (2023).
-
Abraham, G. et al. Genomic risk score offers predictive performance comparable to clinical risk factors for ischaemic stroke. Nat. Commun. 10, 5819 (2019).
-
Lu, X. et al. A polygenic risk score improves risk stratification of coronary artery disease: a large-scale prospective Chinese cohort study. Eur. Heart J. 43, 1702–1711 (2022).
-
Patel, A. P. et al. A multi-ancestry polygenic risk score improves risk prediction for coronary artery disease. Nat. Med. 29, 1793–1803 (2023).
-
Koyama, S. et al. Population-specific and trans-ancestry genome-wide analyses identify distinct and shared genetic risk loci for coronary artery disease. Nat. Genet. 52, 1169–1177 (2020).
-
Said, M. A., Verweij, N. & van der Harst, P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank study. JAMA Cardiol. 3, 693–702 (2018).
-
Rutten-Jacobs, L. C. et al. Genetic risk, incident stroke, and the benefits of adhering to a healthy lifestyle: cohort study of 306 473 UK Biobank participants. Brit. Med. J. 363, k4168 (2018).
-
Khera, A. V. et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N. Engl. J. Med. 375, 2349–2358 (2016).
-
Rothman, K. J., Greenland, S. & Walker, A. M. Concepts of interaction. Am. J. Epidemiol. 112, 467–470 (1980).
-
Khera, A. V. et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat. Genet. 50, 1219–1224 (2018).
-
Martin, A. R. et al. Human demographic history impacts genetic risk prediction across diverse populations. Am. J. Hum. Genet. 100, 635–649 (2017).
-
Dugani, S. B. et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident coronary heart disease in women. JAMA Cardiol. 6, 437–447 (2021).
-
Tian, X. et al. Association of lipid, inflammatory, and metabolic biomarkers with age at onset for incident cardiovascular disease. BMC Med. 20, 383 (2022).
-
Surakka, I. et al. Sex-specific survival bias and interaction modeling in coronary artery disease risk prediction. Circ. Genom. Precis. Med. 16, e003542 (2023).
-
Han, Y. et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur. Heart J. 42, 3374–3384 (2021).
-
Jacob, M. E. et al. Can a healthy lifestyle compress the disabled period in older adults? J. Am. Geriatr. Soc. 64, 1952–1961 (2016).
-
Chen, Z. et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 40, 1652–1666 (2011).
-
Walters, R. G. et al. Genotyping and population characteristics of the China Kadoorie Biobank. Cell Genom. 3, 100361 (2023).
-
Lv, J. et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J. Am. Coll. Cardiol. 69, 1116–1125 (2017).
-
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
-
Chinese Society of Cardiology of Chinese Medical Association. [Chinese guideline on the primary prevention of cardiovascular diseases]. Zhonghua Xin Xue Guan Bing Za Zhi 48, 1000–1038 (2020).
-
The Joint Task Force for Guideline on the Assessment and Management of Cardiovascular Risk in China. [Guideline on the assessment and management of cardiovascular risk in China]. Zhonghua Yu Fang Yi Xue Za Zhi 53, 13–35 (2019).
-
Dale, C. E. et al. Causal associations of adiposity and body fat distribution with coronary heart disease, stroke subtypes, and type 2 diabetes mellitus: a Mendelian randomization analysis. Circulation 135, 2373–2388 (2017).
-
Chen, G. C. et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 40, 2849–2855 (2019).
-
Zhu, Z. et al. A large-scale genome-wide association analysis of lung function in the Chinese population identifies novel loci and highlights shared genetic aetiology with obesity. Eur. Respir. J. 58, 2100199 (2021).
-
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613 (2010).
-
Sjölander, A. & Vansteelandt, S. Doubly robust estimation of attributable fractions in survival analysis. Stat. Methods Med. Res. 26, 948–969 (2017).
-
Hasbani, N. R. et al. American Heart Association’s Life’s Simple 7: lifestyle recommendations, polygenic risk, and lifetime risk of coronary heart disease. Circulation 145, 808–818 (2022).
-
Rapsomaniki, E. et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 383, 1899–1911 (2014).
-
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 140, e596–e646 (2019).
-
VanderWeele, T. J. Reconsidering the denominator of the attributable proportion for interaction. Eur. J. Epidemiol. 28, 779–784 (2013).
-
Si, J. et al. Chronic hepatitis B virus infection and risk of chronic kidney disease: a population-based prospective cohort study of 0.5 million Chinese adults. BMC Med. 16, 93 (2018).
Acknowledgements
The most important acknowledgement is to the participants in the study and the members of the survey teams in each of the ten regional centres, as well as to the project development and management teams based at Beijing, Oxford and the ten regional centres. This work was supported by the National Natural Science Foundation of China (82192901 (L.L.), 82388102 (L.L.), 82192900 (L.L.) and 823B2090 (D.S.)). The CKB baseline survey and the first resurvey were supported by a grant from the Kadoorie Charitable Foundation in Hong Kong. The long-term follow-up is supported by grants from the National Key R&D Program of China (2016YFC0900500) (Y. Guo), National Natural Science Foundation of China (81390540 (L.L.), 91846303 (L.L.) and 81941018 (J.L.)) and Chinese Ministry of Science and Technology (2011BAI09B01) (L.L.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
L.L. and J.L. conceived and designed the study and contributed to the interpretation of the results and critical revision of the paper for valuable intellectual content. L.L., Z.C. and J.C., as the members of the CKB steering committee, designed and supervised the conduct of the whole study, obtained funding, and together with C.Y., Dianjianyi Sun, Y.P., P.P., L.Y., I.Y.M., R.G.W., H.D., X.C., D. Schmidt and R.S. acquired the CKB data. Dong Sun analysed the data. Y.D. and Dong Sun verified the data. Dong Sun drafted the paper. All authors have read and approved the final paper. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. L.L. and J.L. are the guarantors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Yiqiang Zhan and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Note, Tables 1–10 and Figs. 1–12.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
The China Kadoorie Biobank Collaborative Group. Joint impact of polygenic risk score and lifestyles on early- and late-onset cardiovascular diseases.
Nat Hum Behav (2024). https://doi.org/10.1038/s41562-024-01923-7
-
Received:
-
Accepted:
-
Published:
-
DOI: https://doi.org/10.1038/s41562-024-01923-7