September is healthy aging month, which celebrates aging and focuses on the positive aspects of growing older and how we can stay healthy in body and mind. It is also Suicide Prevention month and that is not a topic we always associate/talk about in regard to older adults.
Life expectancy in Northeast Colorado has increased about evenly with the rest of the U.S., from less than 70 years in 1950 to over 80 years in 2020. Our goal should be to live those extra years
healthy in body and mind, experiencing quality of life as well as length.
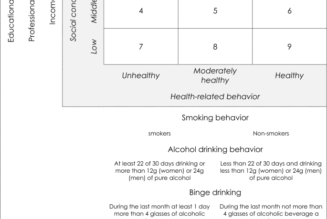
The things that you can do proactively to keep your brain healthy are similar to the things you can do to keep your body healthy: eat a heathy diet, stay active, practice good oral hygiene, and get regular health check-ups. Additionally, pay attention to your mental health and social contacts.
There is strong evidence that loneliness and social isolation can significantly increase a person’s risk of premature death from all causes, a risk level on par with smoking, obesity, and
physical inactivity.
Older adults often experience social isolation and loneliness due to factors such as loss of a spouse, family moving away, loss of self-sufficiency, chronic illness and pain, and hearing loss. Data from multiple sources suggest that social isolation is associated with an almost 50% increased risk of developing dementia, as well as higher rates of depression, anxiety,
and suicide. Some cognitive changes in memory and thinking are a normal feature of aging, however dementia is not an inevitable effect of gettng older. Maintaining a healthy lifestyle and managing related chronic conditions may help decrease the risk of dementia or slow its progression.
In addition to poor diet, lack of exercise, and smoking, known risk factors for Alzheimer’s disease and related dementias include binge drinking, high blood pressure, and diabetes. Brain injury, hearing loss, and depression can also contribute to developing dementia.
Some people notice changes in themselves before anyone else might; for others, friends and family may see changes in memory and behavior. The following are early warning signs:
• Memory loss that disrupts daily life, such as repeating oneself or forgetting the function of an item.
• Difficulty completing familiar tasks like driving or cooking, bathing, dressing, or caring for a pet.
• Confusion with time or place like not being able to understand events as they are happening or losing track of dates, and getting lost.
• Trouble with visual images or spatial relations: having trouble with balance, tripping over items in the home, and inability to judge depth or distance create fall risks that can lead to injuries that further exacerbate decline in health.
• New problems with speech or writing and having trouble finding words.
• Decreased judgement evidenced by not managing money well or becoming the victim of a scam, and increased impulsivity.
• Withdrawal from social activities, and changes in mood or personality.
Depression is also a common, but not normal, feature of aging. Older adults often do not seek treatment for mental health problems or allow their primary care provider to see their accurate mental state. Suicide is one of the leading causes of death in the U.S. and older adults are especially vulnerable due to declines in health and social contact.
Physical, emotional, cognitive, and financial struggles can exacerbate depression to the point it becomes a clinical concern with feelings of sadness and hopelessness that may increase the risk of suicide. Neglecting personal care and medical regimens, giving away treasured items, and preoccupation with death are a few signs that someone may be planning suicide.
We can support the elders in our communities with protective efforts.
• Firstly, understand that depression is not a normal part of aging and that therapy can be beneficial for getting through particularly difficult circumstances.
• Be available – if being physically present isn’t possible, make phone calls and video chats a regular part of your communication with older family and friends.
• If you see signs that concern you, ask direct questions such as “are you considering suicide?” and “do you have a plan?” Help them connect with support systems in the community for mental health and social interaction.
• Follow up. A phone call or card after a trying time can help someone come out the other side of a difficult time. For specific information about older adults and suicide, and ways to support connections and mental health, visit: www.ncoa.org/article/suicide-and-older-adults-what-you-should-know.
If you or someone you know, of any age, is currently in crisis, help is available 24/7 across the country by calling 988 to be connected with a suicide and crisis counselor.