Although people who survive a childhood cancer are at an increased risk of developing and dying from subsequent cancers, as well as heart disease and stroke, they can reduce this increased risk by following a healthy lifestyle, say US investigators.
This message comes from a retrospective analysis of more than 34,000 childhood cancer survivors, which found that 40 years after the initial cancer diagnosis, the cumulative all-cause mortality rate was 23.3%, compared with less than 5% in the general population.
However, following a healthy lifestyle was associated with a 20% reduction in health-related mortality, independent of other factors, the analysis showed. This rose even further, up to a 30% reduction in dying, among individuals who did not have hypertension or diabetes.
The study was published online April 5 in The Lancet.
“We identified that long-term survivors of childhood cancer are experiencing a large number of deaths in excess of what would be expected for the general, aging population,” said first author Stephanie Dixon, MD, MPH, Oncology Department, St. Jude Children’s Research Hospital, Memphis, Tennessee, in a press release.
“These excess deaths are predominantly due to the same leading causes of death as in the general population,” including subsequent cancers, heart disease, cerebrovascular disease/stroke, chronic liver and kidney disease, and infectious diseases, she noted. However, in these childhood cancer survivors they are occuring “at a younger age and higher rate.”

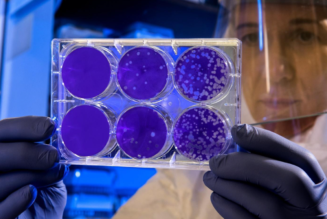
(L-R) Co-author Yutaka Yasui, Ph.D., and senior author Greg Armstrong, MD, MSCE, both of St. Jude Department of Epidemiology and Cancer Control, and lead author Stephanie Dixon, MD, MPH, St. Jude Department of Oncology.
“What was most exciting to see,” Dixon added, “was that, independent of prior treatment exposures and sociodemographic factors, a healthy lifestyle and absence of hypertension or diabetes were each associated with a reduced risk of health-related mortality.”
“This is important because our goal is to extend the life span of survivors and to improve their ‘health span’ as well,” said senior author Greg Armstrong, MD, MSCE, chair of the Department of Epidemiology and Cancer Control at St. Jude.
As such, “the study highlights the importance of encouraging survivors to practice healthy behaviors and maintain good control of cardiovascular disease risk factors,” emphasized co-author Melissa M. Hudson, MD, director of the Cancer Survivorship Division at St. Jude.
Future research should focus on interventions for modifiable lifestyle and cardiovascular risk factors that “may need to be specifically tailored to survivors, with the goal of reducing chronic disease development” and extending their lifespan, the researchers commented.
Late Effects of Treatment
Childhood cancer has a tremendous success rate: in the United States, the 5-year survival rate is now more than 85%.
However, long-term survivors experience excess morbidity and late mortality compared with the general population, both of which are “attributable to late effects of treatment,” the team points out.
Their study focused on individuals who had been diagnosed with cancer before they were 21 years old and who had survived at least 5 years after the cancer diagnosis.
The median age at diagnosis was 6 years, and the most common diagnoses were acute lymphoblastic leukemia (36%), Hodgkin lymphoma (11%), astrocytoma (10%), and kidney tumors (8%).
The team identified 34,230 survivors who had been treated between January 1, 1970 and December 31, 1999, at 31 institutions in the United States and Canada.
They represented approximately 20% of all childhood cancer survivors in the US over the study period. The team notes that 56% of the survivors were male, and the majority (64%) were non-Hispanic white.
The date and causes of death through December 2017 were obtained via linkage to the National Death Index, and cancer treatment information was collated for 21,418 survivors who provided consent. Lifestyle factors — including smoking, alcohol use, physical activity, and unhealthy weight — were graded on a score of 0-4.
Over a median follow-up of 29.1 years, there were 5916 deaths, with 34% attributable to the recurrence or progression of the primary cancer, and 51.2% attributable to other causes, such as subsequent neoplasms, and cardiac, pulmonary, and other health-related causes.
Overall, survivors were at an elevated risk of death vs the general population, at a standardized mortality ratio of 5.6. This ratio peaked at 5-9 years after diagnosis at an 18.1-fold increased risk of death compared with the general population.
Forty years or more from the initial diagnosis, two thirds of the 131 per 10,000 person-years excess deaths from health-related causes were due to the top three causes of health-related death in the general population, the team reports.
This included an absolute excess risk of death from cancer of 54 per 10,000 person-years, an excess risk of heart disease mortality of 27 per 10,000 person-years, and an excess risk of cerebrovascular disease mortality of 10 per 10,000 person-years.
The individual cases of death contributing the greatest excess risk were gastrointestinal cancers (11 per 10,000 person-years), cerebrovascular disease (10 per 10,000 person-years), ischemic heart disease (10 per 10,000 person-years), and valvular heart disease (9 per 10,000 person-years).
The good news is that following a healthy lifestyle was associated with a 20% reduction in health-related mortality vs an unhealthy lifestyle (P = .0020).
Moreover, following even a moderately healthy lifestyle was associated with a 10% reduction in health-related mortality, the researchers noted.
The study was supported by grants from the National Cancer Institute, St. Jude Children’s Research Hospital Cancer Center Support, and the American Lebanese-Syrian Associated Charities. The authors reported no relevant financial relationships.
The Lancet. Published online April 5, 2023. Abstract
For more from Medscape Oncology, join us on Twitter and Facebook