Healthy Eating May Turn Your Gut Bacteria Into Cancer-Fighting Heroes
Recent research out of Dallas and Houston highlights the “science fictionlike” power of your body’s microbiome—and a high-fiber diet.
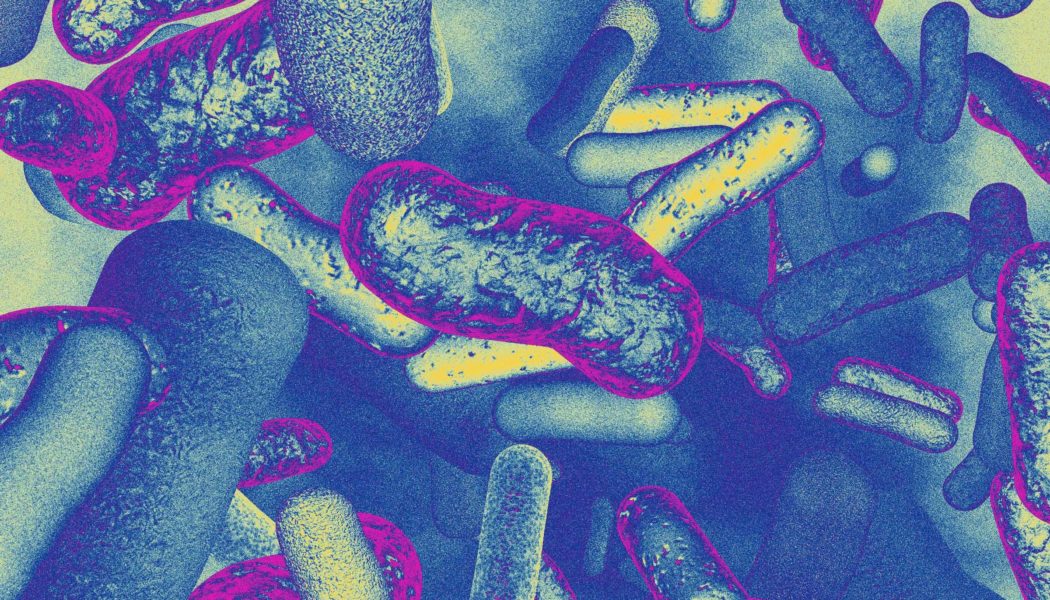
The human body is only one percent human, microbiologists like to say. Each of us plays host to an ecosystem of thousands of species of bacteria, fungi, parasites, and viruses that amount to trillions of microorganisms. Together these compose our microbiome. If you factor in their total genomic content as part of our own, we are 99 percent microbial.
Over the last decade and half, there’s been what Dr. Andrew Koh, a professor of pediatrics and microbiology at UT Southwestern Medical Center in Dallas, calls a “microbiome explosion,” a tremendous increase in research and commercial interest in understanding and manipulating how our microbiome affects our health. The greatest number of microorganisms live in our intestines, but they can be found throughout the body, and they play a major role in our immune system. A host of conditions, ranging from irritable bowel syndrome to depression, has been explored in microbiome research.
A pediatrician specializing in blood disorders, cancer, and infectious disease, Koh explored, in his early work, how bacteria originating in the gut migrated into the bloodstream and caused fatal infections in some of his young, immunocompromised patients. His research focused on neutralizing the threat posed by these so-called “bad bacteria.” But in some of his most recent work, Koh has turned his attention to the “good bacteria.” In a study published earlier this year in the journal Science Immunology, Koh and his colleagues explore what he calls the “science fictionlike concept that bugs in your gut can help you fight cancer.”
The findings shed light on the little-understood process through which, when paired with immunotherapy treatment, some bacteria travel throughout the body to help fend off tumors. Koh’s team is now working to develop treatments that might harness these beneficial bugs. But his work also underscores the importance of what may be an even more powerful cancer-fighting tool, one that’s often overlooked. A growing body of research shows that the most effective way to boost the cancer-fighting power of the gut may be the simplest: a balanced fiber-rich diet can feed these “good bacteria,” making them more robust cancer combatants.
In addition to genetics and environment, diet has long been known to be one of the most important factors determining the kinds of organisms living in a person’s gut. Probiotics—fermented foods and drinks, such as kimchi, yogurt, and pickled vegetables—can add more of the preferred sorts of bugs to our microbiomes. But it’s not just about the type of bacteria, cautions Dr. Jennifer Wargo, a professor of surgical oncology and genomic medicine at the University of Texas MD Anderson Cancer Center in Houston. “It’s about what you’re feeding it that matters,” she says. Fiber-rich foods—beans, fruits, vegetables, whole grains—are sometimes called “prebiotics,” and they promote these “good” gut bacteria.
Studies dating back to 2015 have demonstrated that gut microbes are critical to an immunotherapy response to cancer, but it remained unclear what newly diagnosed patients could do with that information. The problem with asking, “Hey, Doc, what do I eat?” was twofold: not only was there scant research linking diet to cancer prognoses to inform their suggestions, but many physicians aren’t trained in discussing nutrition with patients. “For a long time, I think a lot of oncologists kind of shrugged their shoulders and said: ‘normal, healthy diet’—they didn’t really know what advice to give,” Wargo says.
In the absence of clear medical guidelines, a market for over-the-counter probiotics emerged and promised wide-ranging benefits. But studies by Wargo and others have shown that these probiotics may actually reduce the effectiveness of cancer-fighting treatments. Simply flooding the extraordinarily complex human microbiome with whatever microbes were available in store-bought capsules wasn’t necessarily wise. These findings further complicated our already murky understanding of the microbiome’s role in fighting cancer.
Then, in 2021, Wargo and her colleagues had a breakthrough. They found that melanoma patients who began immunotherapy while maintaining a high-fiber diet responded better to treatments, and survived longer than patients reporting low-fiber diets. “Now we actually have credible data that’s scientifically driven that suggests that a high-fiber diet can actually really boost the immune system and can boost cancer-immunotherapy response,” Wargo says.
At MD Anderson, Wargo’s colleagues, led by Dr. Jennifer McQuade, are conducting a remarkable clinical trial stemming from that 2021 study. The trial aims to better understand how an expertly managed fiber-rich diet affects the gut microbiome and potentially improves cancer outcomes. The researchers are providing every meal and snack, over the course of twelve weeks, to 42 stage III and IV melanoma patients who are receiving immunotherapy. All the while, doctors are tracking how their microbiomes respond. “You take the same bug, and if you feed it McDonald’s, it behaves one way. If you feed it a high-fiber diet, it behaves totally differently,” Wargo says. The study is in its final stages, and Wargo says they have seen some “very striking results.” Findings will be published after the trial has been completed early next year.
Koh, meanwhile, worries that, even with optimized nutritional guidance, some cancer patients won’t be able to stick with the significant dietary changes that could be required. “Diets are great. Diets are probably the most potent way to change the microbiome,” he says. “The problem is, as everybody knows, adhering to diets is hard.”
So Koh is aiming to develop a drug or treatment capable of delivering similar results. In order to do that, he needed to better understand the mechanism through which a healthy gut affects cancer. One question in particular drove Koh and his colleagues crazy: “How does a bug in your gut help you fight cancer that’s not in your gut?” It made sense that these bacteria could help fend off colorectal cancer, for instance, because the bugs are right there, on the scene, to do the fighting. But studies like Wargo’s demonstrated improvements in patients with skin cancer, affecting an entirely different part of the body.
From his earlier research, Koh knew that, under certain conditions, the movement of bacteria in the gut through the rest of the body was often facilitated by the lymph nodes. He also knew that immune checkpoint inhibitors—one form of immunotherapy for cancer patients—caused the lymph nodes to swell. He wondered whether that inflammation could be allowing the bacteria in, and thereby acting as a conduit to fight cancer in other parts of the body. He and his colleagues used mice with melanoma tumors to test and confirm this theory. They also found that antibiotics, which kill off bacteria in the body, diminished the effect of immunotherapy by reducing the number of bugs available to help fight tumors.
“This is yet another potential way that we can utilize and modify the microbiome to hopefully benefit patients in a very real way,” says Dr. Brooks Cash, chief of gastroenterology, hepatology, and nutrition at the University of Texas Health Science Center at Houston. In his own practice, Cash, who had no role in the studies by Koh or Wargo, often advises patients on gut health and the microbiome.
Wargo was likewise impressed that Koh’s study was able to demonstrate a path through which gut microbiota travel the body and induce anti-tumor responses. Still, Cash and Wargo emphasize that we shouldn’t read too much into a process that works in mice but hasn’t yet been demonstrated in humans. “I think this is one way that these bugs in the gut can shape the immune system, but it’s not the only way,” Wargo says. “We haven’t answered all the questions yet. We still need to study this better.”
Nevertheless, Koh started a biosciences company to take this knowledge and develop a “druggable way to really optimize your anti-tumor [immune] response.” He and his team are working on a gut microbiota therapy that can be administered through injection or IV. It’s meant to be paired with immunotherapy and to “skip the gut,” delivering beneficial bacteria directly to the tumor or tumor-draining lymph nodes. Koh hopes to publish more findings this year, then move on to human trials.
Even if the exact contours of the microbiome’s role in fighting cancer remain undetermined, Koh says that it’s “mind numbing” how much we’ve learned about the microbiome in just the last couple of decades. He’s optimistic that the field will continue to progress. “I hate to use the cliche,” Koh says, “but it’s really the tip of the iceberg.”
Despite all the recent advances, and all the mysteries that remain, Wargo says the simplest prescription for patients may still be the best. Those who have plant-based, high-fiber diets see better cancer prognoses, lower incidence of heart disease, and a broad array of improved health outcomes. “We should all be doing what our moms told us,” she explains. “Eat better, exercise, get more sleep.”