Cognitive function was better for older adults with healthy lifestyles even if they had Alzheimer’s or other dementia-related pathologies, autopsy data showed.
A 1-point increase in a healthy lifestyle score was associated with better cognitive performance proximate to death (β=0.216, P<0.001), reported Klodian Dhana, MD, PhD, of Rush University Medical Center in Chicago, and co-authors.
After adjusting for beta-amyloid load, healthy lifestyle scores remained independently associated with cognition (β=0.191, P<0.001), the researchers reported in JAMA Neurology.
Similarly, scores were independently associated with cognition after adjusting for phosphorylated tau tangle pathology (β=0.196, P<0.001) or global Alzheimer’s disease pathology (β=0.193, P<0.001). Lifestyle scores ranged from 0 to 5 points, with higher scores indicating a healthier lifestyle.
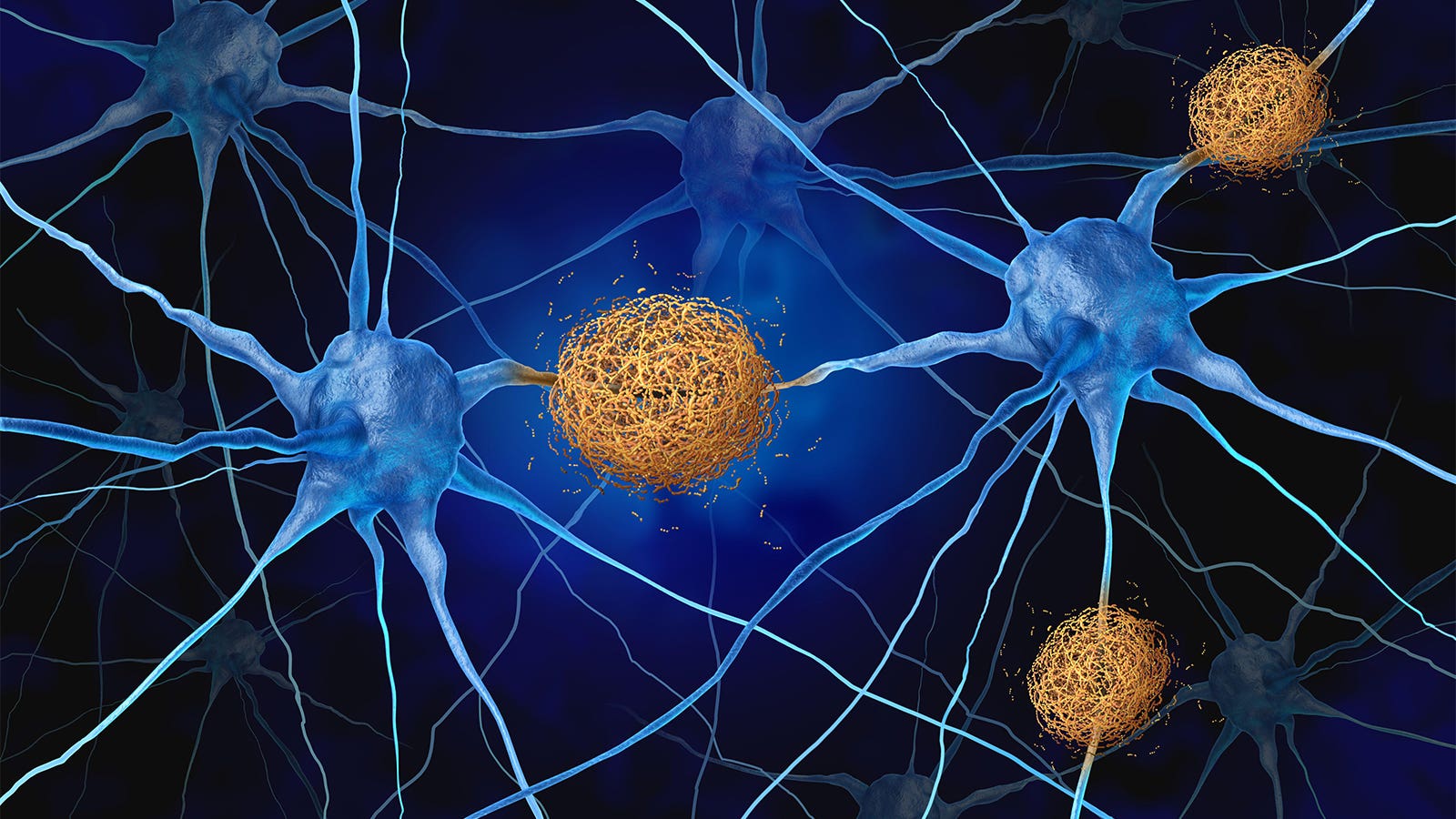
“There are a lot of epidemiological studies, including ours, supporting the role of lifestyle in dementia risk,” Dhana told MedPage Today. “However, as individuals age, there is a progressive accumulation of dementia-related brain pathologies such as beta-amyloid, which raises the question of whether the lifestyle is associated with cognition independently of dementia-related brain pathologies.”
In 2020, the Lancet Commission reported that up to 40% of dementia cases may be prevented or delayed by modifying 12 risk factors, but whether a healthy lifestyle can boost “cognitive reserve” — the ability to preserve cognition despite brain pathology — isn’t clear.
This study may help researchers better understand how modifiable risk factors are associated with dementia, noted Yue Leng, PhD, and Kristine Yaffe, MD, both of the University of California San Francisco, in an accompanying editorial.
“Over the past decade, studies have identified an increasing number of novel risk factors for dementia and have begun to uncover the mechanisms through which these modifiable risk factors could impact cognitive aging and prompted multidomain interventions,” Leng and Yaffe wrote. “Despite this ongoing progress, critical questions remain to be addressed regarding the mechanistic pathways linking modifiable risk factors and cognitive aging and the directionality of this link.”
This study “is one of the first to harness brain pathology to investigate these mechanisms and is a crucial step forward in addressing these important questions,” the editorialists pointed out. “There is an urgent need for more well-designed randomized clinical trials to pave the way for dementia risk reduction in the era of precision medicine.”
Dhana and colleagues used data from the Rush Memory and Aging Project, a longitudinal study with up to 24 years of follow-up and autopsy data. The researchers included 586 decedents with dietary and lifestyle data, cognitive testing proximate to death, and postmortem findings. Most decedents (70.8%) were female, and the mean age at death was 90.9 years.
Lifestyle factors were assessed annually and considered low risk or “healthy” based on MIND diet adherence, late-life cognitive activity scores, no current smoking, moderate or vigorous exercise activities for at least 150 minutes a week, and light to moderate alcohol intake. The mean of each lifestyle factor from enrollment to study until death was computed to help reduce reverse causation.
Cognitive function was measured annually with 19 tests. The researchers used global cognitive scores before death in this analysis; the median time between the last cognitive assessment and death was 0.8 years.
Postmortem beta-amyloid was evaluated at multiple brain regions, as was phosphorylated tau tangle density. Atherosclerosis, arteriolosclerosis, microinfarcts, macroinfarcts, cerebral amyloid angiopathy, Lewy body disease, hippocampal sclerosis, and TAR DNA-binding protein 43 (TDP-43) also were assessed.
A higher lifestyle score was associated with lower beta-amyloid load in the brain (β = −0.120, P=0.003), the researchers reported. The overall estimated association of lifestyle score on cognition was 0.216, with an indirect association through a beta-amyloid load of 0.025 (P=0.008), or 11.6%.
Excluding people with poor cognition at baseline or clinical Alzheimer’s dementia proximate to death attenuated the estimates, but links between lifestyle scores and cognition remained statistically significant and independent of common brain pathologies.
The findings suggest that lifestyle may provide cognitive benefits even for people who have begun to accumulate dementia-related pathologies, Dhana noted. “However, we must note that this is an observational study using pathological data at autopsy, and additional clinical studies are needed to support these findings,” he said.
The study sample consisted mainly of white volunteers who agreed to annual evaluations and postmortem organ donation, limiting the generalizability of the findings to others, the researchers acknowledged. In addition, lifestyle factors were self-reported.
Disclosures
The study was supported by grants from the National Institute on Aging.
Dhana reported grants paid to his institution from the Alzheimer’s Association. Co-authors reported relationships with the Alzheimer’s Association, the Michael J. Fox Foundation for Parkinson’s Research, Eisai, and Alzheimer’s and Dementia.
Leng and Yaffe reported receiving grants from the National Institutes of Health.
Primary Source
JAMA Neurology
Source Reference: Dhana K, et al “Healthy lifestyle and cognition in older adults with common neuropathologies of dementia” JAMA Neurol 2024; DOI: 10.1001/jamaneurol.2023.5491.
Secondary Source
JAMA Neurology
Source Reference: Leng Y, Yaffe K “Harnessing brain pathology for dementia prevention” JAMA Neurol 2024; DOI: 10.1001/jamaneurol.2023.5490.









