“How did we get here?”
That was one of the first questions asked by Rainelle Gaddy, PharmD, MS, MBA, strategy advancement lead at Humana, during her session on health care inequities in the United States. The session was held at the Pharmacy Quality Alliance (PQA) 2023 Annual Meeting, which took place May 10-12, 2023, in Nashville, Tennessee.
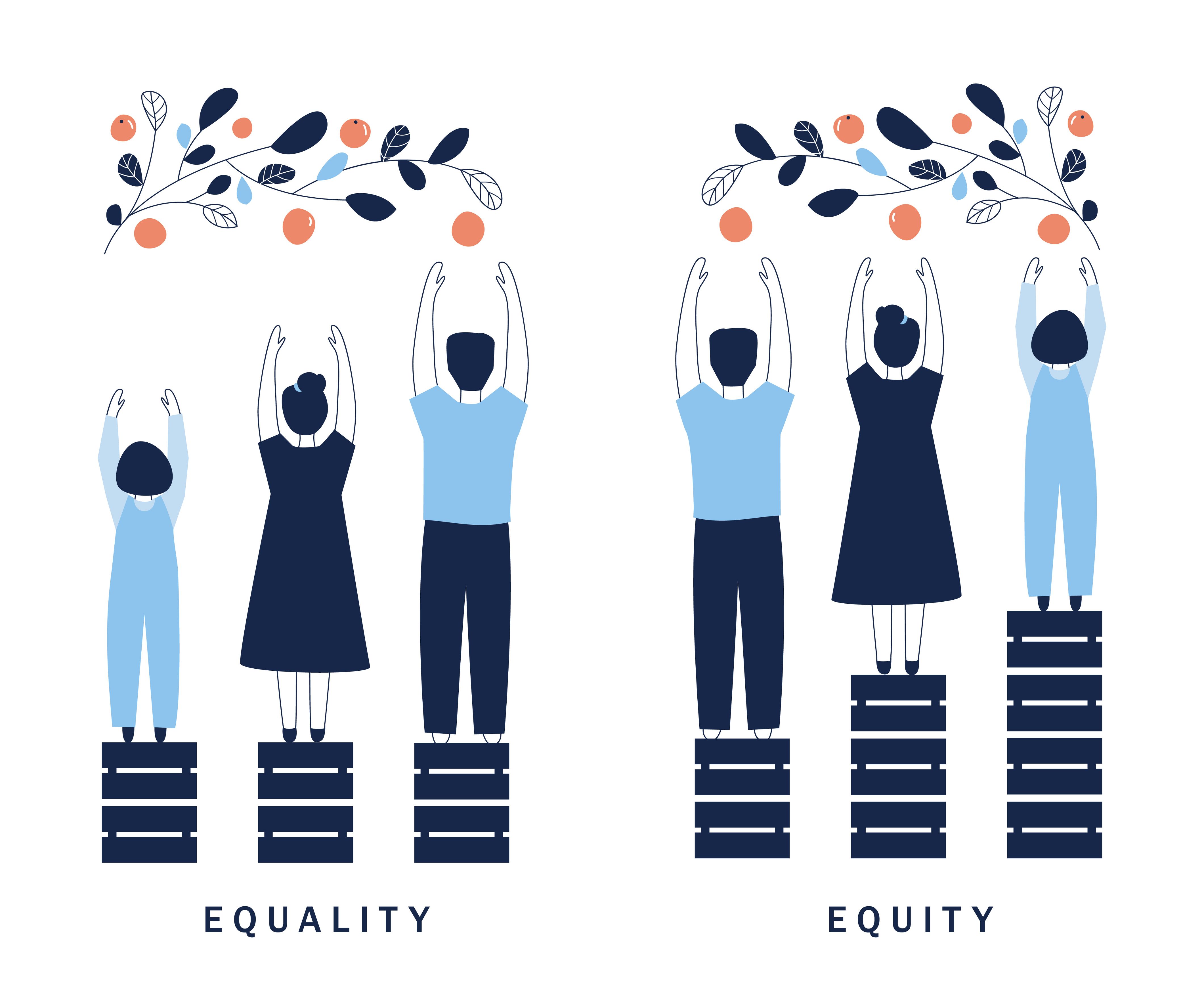
Gaddy began to answer her question by reviewing the factors resulting in health inequities, which she defined as unfair and avoidable differences in health status.
First are upstream determinants—namely discrimination, racism, and poverty. Gaddy said these upstream determinants are largely rooted in beliefs that some groups are superior to others, which can result in discriminatory policies, which can further lead to inequitable distribution of power, resources, and money, or exclusion of certain groups.
These upstream determinants then lead to midstream determinants, which include but are not limited to food insecurity, unsafe housing, education, health care inaccessibility, low quality health care, income inequality, and unemployment.
“For example, housing policies that started in the 1930s discouraged investment in Black, immigrant, and low income neighborhoods,” Gaddy recalled, explaining the shift from upstream to midstream determinants. “Because these neighborhoods were designated as not being credit worthy, this prevented Black, indigenous, and people of color from obtaining mortgage loans. This resulted in the disinvestment of critical infrastructure in these neighborhoods.”
These living conditions and other factors then lead to downstream determinants, which are essentially medical conditions that could have been otherwise avoidable. For example, poor living conditions may contribute to health issues like asthma, while stress-related hypertension due to unemployment may lead to hospitalization. These downstream factors are influenced by midstream determinants and the discriminatory policies in place.
As Gaddy explained, Humana is committed to advancing health equity and has taken significant steps to promote equitable access to pharmaceutical care, with a focus on improving access to care, enhancing the quality of care, and addressing barriers to healthy living.
“It’s going to be key to understand that this is not a sprint, it truly is a marathon,” Gaddy said.
One of Humana’s key initiatives is the establishment of the Pharmacy Health and Equity Council, aimed at embedding health equity into their business products and services. To improve access to care, Humana plans to expand health insurance coverage for members with the greatest needs, minimizing issues related to transportation, cost barriers, and geographical constraints. They are also developing models of integration to address social needs and ensure culturally competent care, ultimately improving the overall quality of care for members.
From a pharmacy benefit manager (PBM) perspective, in order to make meaningful advancements in pharmaceutical care, Humana has identified 5 key areas of focus: formulary development; equitable benefits plans; clinical programs addressing physical, social, and behavioral needs; improved medication access; and thought leadership through collaboration and the sharing of best practices.
Education, data analytics, and reporting also play a crucial role in Humana’s efforts, as they are investing in education and cultural competencies across the organization to promote health equity awareness and advocacy. They are also utilizing data analytics and research to monitor and report the progress of their initiatives, both internally and in external forums.
To further add to the list of efforts, Humana is also implementing enhancements throughout their therapeutic continuum, targeting disease states and medications to align with their formulary planning. Health literacy is also a priority, ensuring clear and concise communication with members, including coverage determination letters. Through this approach, frontline health care workers are empowered and trained to understand and address the diverse needs of Humana’s member population, and bilingual associates are available to engage with members effectively.
Recognizing the impact of social determinants of health on medication adherence, Humana has also conducted a pilot program that involved pharmacists screening Medicare members for social needs and providing support in partnership with community organizations. This initiative aimed to address social needs and improve medication adherence among individuals facing social disparities.
A few of the major lessons Humana learned from this pilot program were the importance of education, understanding the culture of equity shift and that gaps exist, and that cross collaboration is critical to truly achieve health equity.
“When there’s a generation of data and best practices that are shared in a diverse manner, we’ve got to understand and know everything we do is going to be centered around that patient, that member; they are the heart of everything that we do,” she continued. “Because we understand and know that, it is going to be key to have collaboration amongst providers, the payers, health care systems, community, as well as national organizations such as [PQA] as we move forward.”
For PBMs to advance health equity, Gaddy explained that it is crucial to focus on incorporating social determinants of health into a comprehensive model. Understanding the unique needs of the population and prioritizing them is key and utilizing data to identify opportunities and integrating behavioral, social, and physical health services into primary care can create a proactive system that emphasizes prevention and promotion.
Mobilizing and collaborating with community and industry relationships is the next essential step, with Gaddy saying that effective change requires collective action rather than “just 1 person moving and operating in their own silo.” By leveraging collaborative efforts, PBMs can drive impactful transformations.
Achieving balance is the third vital component. According to Gaddy, PBMs should strive for a balance between financial considerations and outcomes that address the holistic wellbeing of individuals, and recognizing the influence of individual factors is crucial for making meaningful progress in advancing health equity through PBM programs.
“There comes a point where we need to stop just pulling people out of the river,” Gaddy shared, reciting a quote by Desmond Tutu, former South African Anglican bishop. “We need to go upstream and find out why they’re falling in.”