Starting in late 2019 to early 2020, the novel SARS-CoV-2 virus rapidly spread from country to country and caused the worldwide COVID-19 pandemic that has continued into 2022. Most patients are asymptomatic or have mild disease. However, a considerable percentage of people have extensive pneumonia that can advance to hypoxemic respiratory failure, shock, multiple organ dysfunctions, and death [21]. COVID-19 vaccinations are thought to be extremely important to prevent and control COVID-19 because immunization is one of the health strategies that works the best and most affordably to avoid infectious diseases, Case series of vaccine-breakthrough infections also have been reported by variants of concern “VOCs,” such as the delta variant [22].
To our knowledge no previous study has correlated HEI-2015 with infectious diseases. High scores on the HEI-2015 suggest a healthy eating pattern that is high in fruits and vegetables, whole grains, dietary fiber, lean proteins, and unsaturated fatty acids and low in refined grains, sodium, added sugars, and saturated fats. Our study aim was to assess the effects of healthy diet and physical activity on COVID-19 disease outcomes examining correlation among the HEI-2015 and physical activity GPAQ with the disease course and recovery in mild- and moderate COVID-19 patients.
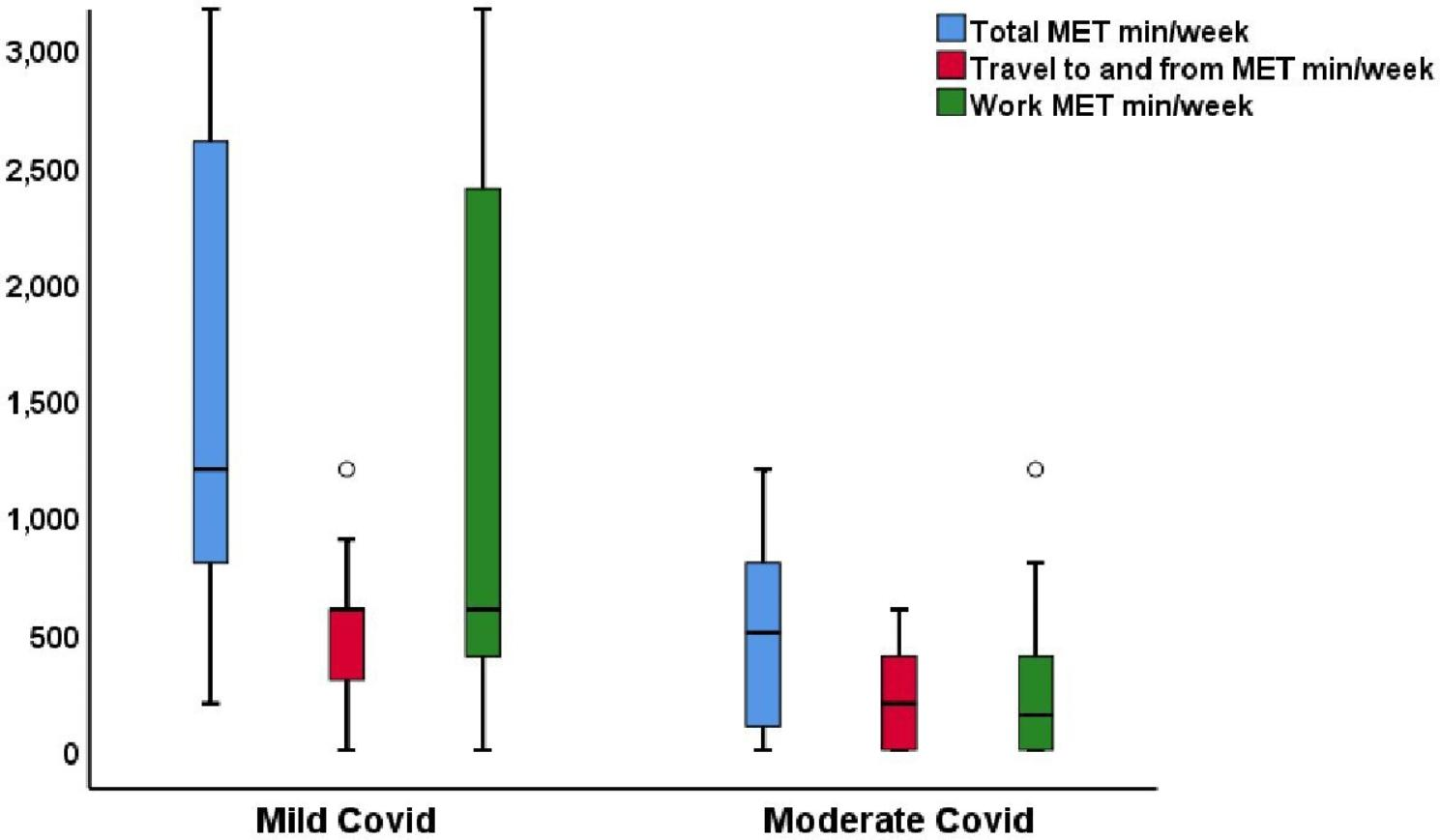
The main findings in our study were as follows: the median total HEI score was higher in the patients with mild COVID-19 than in those with moderate COVID-19. There was a significantly positive correlation among all COVID-19 patients between the lymphocyte count and HEI-2015 (p = 0.005). The GPAQ results showed that, 92.1% of the patients with mild COVID-19 patients were physically active (≥ 600 METs-min/week), compared to 50% of moderate COVID-19. The total METs-min/week was significantly and positively correlated with the lymphocytic percentage (p = 0.003) and negatively correlated with the neutrophil lymphocyte ratio (, p = 0.009) in patients with moderate COVID-19. The HEI-2015 was the main factor affecting the severity of COVID-19 disease, as shown by the finding that for every unit increase in the HEI-2015 score, there was about a 64% reduction in the risk of having moderate COVID-19.
A prior study on influenza patients showed that a good diet decreased the patients’ hospitalization rate, which is evidence that a healthy food pattern likely reduces the risk of severe COVID-19 [23]. On the other hand, alterations in some inflammatory markers caused by a bad diet may result in systemic inflammation [24].
A properly balanced diet, rich in all macronutrients and micronutrients, affects the functioning of the immune system positively. Enriched foods or a balanced diet including vitamins and minerals C, A, E, zinc, and vitamin D contribute to fighting and preventing the proliferation of SARS-CoV-2 virus cell particles and minimizing mortality and complications resulting from COVID-19 disease. The relationships described are important in that they also have their role in post- COVID prophylaxis and affect the building of lifelong immune reserves protecting against repeat infections and the development of a dangerous course of infection [25].
Our study assessed dietary habits 1 year prior to infection instead of what the patients recalled eating over the most recent 24-hours period because anorexia, fever, and gastrointestinal disturbance during infection can change the quality and quantity of the food choices by the patients. Besides, ensuring that the healthy lifestyle is maintained for an individual over one year gives a clue that micro and macro nutrients needed for proper immunity are provided. Analysis of the FFQ revealed that; saturated fat, refined grains, and sugar were consumed in significantly higher amounts by patients with moderate COVID-19 than those with mild disease. The patients with mild COVID-19 were found to have significantly higher ingestion of the total vegetables, greens, and beans than those with moderate COVID-19, and they had non-significantly higher consumption of total fruits, whole fruits, and seafood and plant protein. Consumption of dairy products, fatty acids, whole grains, and total protein were more or less similar between the two COVID-19 groups.
A previously published study that assessed the nutritional habits of COVID-19 patients found that individuals who consumed less fruit and poultry in their regular diets had more severe forms of the illness, and patients who drank more black tea appeared to have a higher chance of developing severe illness [26]. Our study findings agree with those of a previous study on respiratory viral infection involving influenza patients, where inactivity and low fruit and vegetable diet were linked to a higher likelihood of influenza hospitalization [23].
The present study results regarding the individual items of added sugar, total vegetables, greens and beans within the HEI- 2015 score, are in agreement with our previously published work on 200 COVID-19 patients who were evaluated using our novel ESSAP score (Exercise, Sugar consumption, Sleeping hours, Antibiotics, and Prebiotics consumption), which revealed that daily consumption of prebiotic-containing foods and sugar consumption of less than two teaspoons resulted in a milder disease and quick virus clearance [27].
A significantly fair positive correlation was observed among all COVID-19 patients between the lymphocyte count and HEI-2015 (p = 0.005). The total HEI-2015 score was positively correlated with serum ferritin among the patients with mild COVID-19 (p = 0.047).
Good dietary quality as measured by the HEI-2015 was associated with lower CRP and interleukin (IL)-6 concentrations, as well as white blood cell counts and its constituents. Significant relationships were also found for CRP, neutrophils, lymphocytes, and their neutrophil: lymphocyte ratio with total fruit intake in a previous study that examined the relationships between the HEI-2015 score and a range of inflammatory biomarkers in a cross-sectional sample of 1989 men and women There were no connections discovered between dairy, total protein meals, refined carbohydrates, or sodium and any inflammatory biomarkers [28].
Most of our mild patients where physically active (92.1%), and 73.7% of them showed moderate physical activity compared with only 50% of the patients with moderate COVID-19 than in the patients with mild COVID-19 (p < 0.001), whereas sedentary behavior was significantly higher in the patients with moderate COVID-19 than in the patients with mild COVID-19 (p = 0.014).
Physical activity has been investigated and reported to have a negative impact on severe COVID-19 results. The odds of hospitalization were 2.26 times higher for COVID-19 patients who continuously undertook sedentary behavior during the two years prior to the pandemic (OR 2.26; 95% CI: 1.81–2.83) than for COVID-19 patients who consistently met physical activity recommendations. Additionally, those who were consistently inactive had higher risks of being admitted to an intensive care unit (OR 1.73, 95% CI 1.18–2.55) and dying (OR 2.49, 95% CI 1.33–4.67) [29]. Even low-to-moderate intensity exercise decreased the likelihood of acquiring severe COVID-19 symptoms, which are linked to increased mortality [30].
Physical inactivity is typically linked to increased BMI and a higher likelihood of developing diabetes, both of which are comorbidities linked to negative COVID-19 results [31]. However, it has been discovered that a sedentary lifestyle increases mortality of COVID-19 hospitalized patients regardless of other risk variables (hazard ratio 5.91 (1.80-19.41); p = 0.003) [32].
A previous study involving 206 COVID-19 patients found that: patients with lower METs min/week not only developed a more severe form of the disease, but also demonstrated a statistically significant relationship between the duration of signs and symptoms and level of moderate to vigorous physical activity [26].
Our study revealed a significant moderate-to-good positive correlation between total METs-min/week and lymphocytic percentage (r = 0.53, p = 0.003) in addition to a significantly fair negative correlation between total METs-min/week and the neutrophil: lymphocyte ratio (r = -0.47, p = 0.009) among patients with moderate COVID-19.
The immune system is greatly changed by regular exercise. While prolonged or high-intensity exercise without adequate rest might cause lower cellular immunity, which can increase the propensity for infectious diseases, moderate-intensity exercise boosts cellular immunity [33]. Epidemiologic research have consistently found lower levels of white blood cell counts, CRP, IL-6, IL-18, tumour necrosis factor-alpha, and other inflammatory biomarkers in individuals who engaged in more physical activity and fitness [34, 35].
Finally, it appears that the effects of nutritional habits and physical activity are crucial factors related to COVID-19 disease severity. During the COVID-19 pandemic it is important to stay active and to exercise regularly in addition to maintaining healthy dietary habits, not only as a way to maintain good health, but especially to increase immunoprotective and immunoregulatory activity.
Nevertheless, there are limitations to our study, the number of patients was small to examine the combination/interaction of HE and PA in the explanation of COVID-19 outcomes, there is some sort of recall bias and subjectivity in FFQs as some patients may exaggerate or even underestimate what they eat for social and psychological factors, there was an unequal distribution in the disease severity groups, and there were no patients with severe COVID-19. Future studies in a greater number of patients with a wider range of COVID-19 severity may provide results that are more broadly applicable.
Conclusions
Healthy eating habits and Physical activity might correlate with COVID-19 disease severity and the inflammatory markers.
Recommendations
Individuals should perform a regular variable intensity exercise on a daily basis and strive for a high HEI-2015 by consuming healthy nutrition to help improve immune responses, which will provide greater protection against exposure to the SARS-COV-2 virus and reduce the risk of developing severe COVID-19.