Anderson Francisco Vilchez-Chavez,1,* Eidi Bernal Altamirano,1,* Wilter C Morales-García,2 Liset Sairitupa-Sanchez,3 Sandra B Morales-García,4 Jacksaint Saintila5
1Public Health Postgraduate Unit, Peruvian Union University, Lima, Peru; 2School of Medicine, Faculty of Health Sciences, Peruvian Union University, Lima, Peru; 3School of Psychology, Faculty of Health Sciences, Peruvian Union University, Lima, Peru; 4Faculty of Pharmacy and Biochemistry, Cientifica Del Sur University, Lima, Peru; 5School of Medicine, Faculty of Health Sciences, Señor de Sipan University, Chiclayo, Peru
Correspondence: Wilter C Morales-García, School of Medicine, Faculty of Health Sciences, Peruvian Union University, Lima, Peru, Email [email protected] Jacksaint Saintila, School of Medicine, Faculty of Health Sciences, Señor de Sipan University, Km 5, Carretera a Pimentel, Chiclayo, Lambayeque, 14001, Peru, Email [email protected]
Background: Healthy habits contribute to the prevention of diseases and, therefore, improve the health-related quality of life of people. However, stress is one of the main risk factors associated with serious health problems in the individual. Therefore, the literature suggests a relationship between healthy habits, stress, and health-related quality of life.
Objective: To assess the factors of healthy habits and stress associated with health-related quality of life in a Peruvian adult population.
Methods: A cross-sectional study was conducted with a sample of 540 Peruvian citizens aged between 18 and 60 years. A questionnaire was applied on the Google Forms platform to be completed online, using the “Healthy Lifestyle Questionnaire” and the PSS-4 to assess healthy habits and stress, respectively. Health-related quality of life was evaluated using the EuroQol-5D.
Results: In the multivariate analysis, stress was the most associated factor with quality of life. Physical activity, drug consumption, tobacco consumption, rest habits, and a balanced diet were healthy habits associated with quality of life.
Conclusion: Physical activity, rest habits, and a balanced diet improve health-related quality of life, while drug or tobacco consumption and stress are associated with a lower health-related quality of life.
Introduction
Healthy habits are a set of conscious, collective, and repetitive behaviors aimed at improving the physical, social, and mental health of people.1 Unhealthy habits are one of the main causes of the increase in the rates of non-communicable diseases in Peru.2 In fact, 14.9% and 62.2% of the Peruvian population over 15 smoked at least one cigarette and consumed some alcoholic beverage in the last 12 months, respectively.3 Only 10.5% of Peruvians over the age of 15 consumed at least 5 servings of fruits and/or vegetables per day.3 In addition, the average daily consumption of fruit servings by people in this same age group was 2.0 servings, which is lower than the amount recommended by the World Health Organization (≥ 5 servings of fruits and vegetables per day).3,4 On the other hand, less than 12% of the Peruvian population performs physical activity exclusively for the benefit of their health, which is worrying because not performing these healthy practices can favor the appearance of non-communicable diseases, such as arterial hypertension, obesity, osteoporosis, diabetes and even various types of cancer, among others.3
In contrast, a healthy and balanced diet can improve health-related quality of life and decrease the risk of mortality.5,6 The findings of a study found that healthy dietary patterns improve the quality of life of participants.5 Similarly, the results of another study that examined the relationship between dietary patterns and health-related quality of life indicated that greater adherence to healthy dietary patterns, such as the Mediterranean diet, was associated with better quality of life in different aspects, such as physical, mental, and social health.7 On the other hand, unhealthy dietary patterns, such as the Western diet, were associated with poorer quality of life.6 Additionally, in a study he investigated the health-related quality of life in vegetarians and non-vegetarians, the results showed that vegetarians had a better quality of life in terms of physical, emotional, and social well-being compared to non-vegetarians.8 These findings highlight the importance of a healthy dietary pattern in promoting an overall good quality of life.
On the other hand, several studies support the importance of physical activity in promoting a healthy lifestyle, improving quality of life and overall well-being.9–11 The results of a systematic review highlighted that regular physical activity was positively associated with better quality of life, greater psychological well-being, and improved mood.9 In another study conducted on university students, they highlighted that those who regularly participated in sports activities and had a high level of physical activity reported better health-related quality of life compared to students who had lower levels of physical activity.10 Furthermore, this study showed a positive association between sport and physical activity with aspects such as physical health, psychological well-being, vitality, and the general perception of quality of life.10 Considering these findings, it is important to encourage participation in sports activities and promote an active lifestyle to improve the quality of life in the general population.
Likewise, adequate rest, including a sufficient number of hours of sleep, has positive effects on a person’s health-related quality of life, mood, and general well-being. In fact, people who experience compensatory sleep on weekends have a better health-related quality of life compared to those who do not.12 Also, significant positive impacts on physical health, emotional well-being, and vitality are observed in those who achieve adequate sleep during the weekend.12 Another study conducted in university students in northeast China revealed that shorter sleep duration was negatively related to health-related quality of life.11 Consequently, it is important to encourage the adoption of practices that promote adequate sleep, as this can contribute to improving their quality of life.
In addition, it is important to address both the adoption of healthy habits and stress management to improve health-related quality of life.13,14 For example, chronic and prolonged stress can have a negative impact on various aspects of life, including physical, mental, and emotional health, interpersonal relationships, work and academic performance, and overall life satisfaction.15 Excessive stress can contribute to the development of health problems such as cardiovascular disease, sleep disorders, anxiety, and depression.16 Therefore, it is important to manage stress appropriately and adopt effective coping strategies to improve quality of life. By promoting a healthy lifestyle and developing effective strategies to manage stress, one can contribute significantly to the improvement of people’s health and well-being.
The scientific literature has observed a relationship between healthy habits, stress, and health-related quality of life in various contexts.5,6,9–11,15 However, it is important to note that there is a lack of specific knowledge in the Peruvian context. Although research has been conducted in other countries, it is necessary to carry out studies in the Peruvian context to better understand how these factors interrelate and affect the quality of life of the Peruvian population. These studies can provide relevant information to develop health promotion strategies and improve quality of life in the Peruvian context. Therefore, the aim of this study was to determine the relationship between healthy habits and stress with quality of life in Peruvian adults.
Materials and Methods
Study Design and Participants
This study was a descriptive and cross-sectional design that identifies the influence of physical activity, drug use, tobacco use, sleep habits, balanced diet, and stress as predictors of quality of life in the Peruvian population. The individuals who took part in the research came from the three geographical regions of the country: coast, highlands, and jungle. Participants were selected using a non-probability convenience sampling method. In this approach, the individuals who formed part of the sample were selected intentionally and in a manner accessible to the researchers, without following a random selection process; this type of sampling was used due to its convenience and practicality for the study in question. The inclusion criteria were as follows: a) Peruvian nationality, and b) age between 18 and 60 years old. Foreigners residing in Peru were excluded from the study, as well as people with special needs or terminal illnesses. For data collection, Google Form was used to create the survey. Once developed, various communication channels were established with participants, using social networks (eg, Facebook and WhatsApp) and email. Through these means, potential participants were contacted and provided with the link to the online survey.
The sample size was calculated using the G*Power 3.1.9.7 program. The number of explanatory variables in multiple linear regression is 8. For an effect size of 0.10, a statistical power of (1 – ß) 0.90, and a significance level (α) of 0.05 for multiple regression analysis, the minimum sample size required was 199. Possible incomplete data were considered, so 540 validated data were analyzed.
Ethical Aspects
This study received ethical approval from the Ethics Committee of the Universidad Peruana Unión (registration number: 2022-CE-EPG-0000109) and was conducted following the guidelines of the Declaration of Helsinki. All participants were treated in accordance with these guidelines. The privacy and anonymity of the participants was ensured, and informed consent was obtained before starting the research.
Measurement Instruments
The Spanish version of the “Healthy Lifestyle Questionnaire” was used to evaluate healthy habits. This questionnaire has useful properties in adult populations; it consists of 27 items grouped into 7 factors: Balanced Diet (3 items), Respect for meal times (3 items); Sleep habits (3 items); Tobacco use (3 items); Alcohol consumption (5 items); Consumption of other drugs (5 items) and Physical activity (5 items). It shows an adequate structure, acceptable fit indices and high levels of internal consistency in each factor according to McDonald’s Omega coefficient (Balanced Diet = 0.79, Respect for meal times = 0.82; Sleep habits = 0.91; Tobacco use = 0.96; Alcohol consumption = 0.90; Consumption of other drugs = 0.91 and Physical activity = 0.90).17
The “Perceived Stress Scale” (PSS) in its short 4-item version in Spanish was used to evaluate stress. This scale assesses the degree to which people perceive a lack of control in their daily lives. The 4-item version includes two positive and two negative items. The internal consistency values were acceptable (>0.70) based on the calculation of Cronbach’s Alpha and McDonald’s Omega.18
To measure health-related quality of life, the Spanish EuroQol-5D was used, which is a generic health-related quality of life measurement instrument that can be used both in relatively healthy individuals (general population) and in groups of patients with different pathologies. The EuroQol-5D consists of five domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). These can be classified into three levels of severity (no problems, some or moderate problems, and extreme situations).19 It also presents good internal consistency values (Cronbach’s Alpha = 0.65).20
Statistical Analysis
In this study, descriptive statistics were used to summarize the characteristics of the participants in terms of percentage and mean with standard deviation (SD). Possible gender differences were explored through a chi-square test of independence for categorical variables. Additionally, to evaluate the relationship between the study variables, the Pearson correlation coefficient was calculated.
Subsequently, a multiple linear regression analysis was performed to identify how much explanatory power healthy habits, tobacco consumption, drug use, physical activity, sleep habits, balanced diet, and stress have on health-related quality of life. Additionally, the demographic characteristics of the participants were adjusted as dummy variables to take into account their influence on the results. The data were analyzed using the open-source software R 4.1.1.
Results
Descriptive Analysis
A total of 540 Peruvian adults participated in the study with an age range of 18 to 60 years (Mean=30.3, Standard Deviation=9.1). Table 1 shows that the distribution of marital status and income level does not present significant differences between women and men (p > 0.05). However, significant differences (p < 0.01) were found in the proportions of the categories of educational level, religion, and origin between women and men.
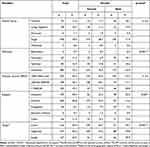 |
Table 1 Distribution of Sociodemographic Variables |
Preliminary Analysis
Table 2 presents the correlation matrix showing a series of variables related to health and well-being, along with the means (M) and standard deviations (SD) for each of them. In this table, the internal consistencies alpha was also observed to be between the values of 0.08 and 0.62.
 |
Table 2 Mean, Standard Deviation, and Correlations |
Multivariate Analysis
The multivariate regression analysis presents the results of a multiple regression analysis, where quality of life is used as the dependent variable and various other variables as independent variables (Table 3). Thus, physical activity (β = 0.043), rest habits (β = 0.056), and a balanced diet (β = 0.051) have a significant positive effect on quality of life (p < 0.05). On the other hand, drug use (β = −0.054), tobacco consumption (β = −0.049), stress (β = −0.130), and being married have a significant negative effect on quality of life (p < 0.05). Incomes greater than 1000 soles (β = 0.202) and greater than 3000 soles (β = 0.385) also have a significant positive effect on quality of life. The other independent variables do not have a significant effect on the dependent variable. The variables analyzed in this model significantly explain 36.9% of the variability of life satisfaction (R2 = 36.9, F = 24.62, p = <0.001).
 |
Table 3 Multivariate Analysis of Related Factors in Quality of Life |
Discussion
In this study, the health status of a representative sample of the Peruvian adult population was explored using the EuroQol-5D. Partial evidence was found to support the hypothesis about the association between healthy habits and health-related quality of life. The combination of different healthy habits factors, such as a balanced diet, regulated physical activity, and effective stress management, has a positive impact on health behavior and quality of life.21 The practice of healthy habits and food security in the population improves quality of life and prevents adverse outcomes for mental and physical health.22
According to our findings, a negative association was observed between being married and health-related quality of life. This finding suggests that married people may experience higher levels of responsibility, which in turn, may result in burnout and stress, negatively impacting their quality of life.23,24 In contrast, a significant positive association was found between income above 1000 soles and quality of life. These results support existing evidence suggesting that low socioeconomic status may contribute to inequality in quality of life. This can be attributed to factors such as lower educational level, more precarious housing conditions, and a greater occupational burden in the household, which can have a negative impact on perceived quality of life.23–26
In the current study, it was also shown that physical activity had a positive effect on the quality of life of the participants. The impact of physical activity on health-related quality of life has been amply demonstrated in several studies in adult populations.27–29 In fact, numerous studies have consistently demonstrated the positive impact of physical activity on health-related quality of life in adult populations.10,30,31 Evidence supports that regular physical activity is associated with a number of physical, mental, and social health benefits, which, in turn, result in a better quality of life.10,30,31 Therefore, promoting regular participation in physical activities appropriate to individual abilities and preferences is critical to improving overall health and well-being. The COVID-19 pandemic has had a significant impact on health-related quality of life due to social distancing measures and restrictions imposed to contain the spread of the virus.16,32 These measures have led to a decrease in physical activity and a greater sedentary lifestyle in a large part of the population, which has had a negative impact on health and well-being.16,33 Confinement and restrictions have limited opportunities for outdoor physical activity, such as walking, running, or sports.34 In addition, the closure of gyms and sports centers has made it difficult to access facilities to stay active. As a result, many people have experienced a more sedentary lifestyle; this decrease in physical activity has had multiple negative effects on health-related quality of life.35,36
On the other hand, drug and tobacco consumption was negatively related to health-related quality of life in adults. As other studies have shown, the consumption of harmful substances, especially drugs and tobacco, is associated with a deterioration of health-related quality of life in adults.37–39 These substances can contribute to serious public health problems, such as chronic addictive disorders and cardiovascular diseases, which can negatively affect current and future quality of life.40 However, some authors have pointed out that factors such as low income, low education levels, and depressive symptoms can predict drug and tobacco consumption.41
An important result that emerges from this research is the positive association between having adequate rest habits, such as sleeping 7 to 8 hours, with health-related quality of life. These results are consistent with other studies conducted on adult populations, where adequate rest had a positive impact on health-related quality of life.11,12,42 Both lack of sleep and excessive sleep have been found to be associated with significant impairment in health-related quality of life in adults with chronic diseases;43 with negative effects on physical health, mood, mental health, and chronic disease management.11,12 In addition, sleep alterations are closely related to mental health and can be a risk factor for cognitive decline compared to adults with good sleep quality.44,45 Therefore, maintaining adequate sleep duration is important for preserving and improving health-related quality of life in adults.
In the present study, a positive correlation was observed between following a balanced diet and a higher health-related quality of life. This is consistent with previous research supporting the idea that adopting healthy eating habits and following balanced diets can improve quality of life in terms of physical and mental well-being.5,6,46,47 In fact, a balanced diet that includes a variety of healthy foods provides the body with nutrients necessary for optimal functioning, preventing chronic diseases,8 maintaining a healthy weight,48 and psychological benefits,47 such as improved mood and self-esteem.49 In fact, some studies have suggested that certain nutrients, such as omega-3 fatty acids and B vitamins, may have a beneficial effect on mental health.47 In addition, healthy eating patterns are associated with a significant reduction in the risk of mortality from any cause, highlighting the importance of maintaining a healthy diet throughout life.32,50,51 However, inappropriate eating behaviors are related to a significant decrease in health-related quality of life.52
Finally, a relationship was found between perceived stress and health-related quality of life. Other studies have demonstrated that stress has a direct negative impact on health-related quality of life.30,53 Moderate levels of perceived stress are correlated with multiple health indicators, such as loneliness, alcohol consumption, and the presence of anxiety and depression symptoms, and are negatively associated with quality of life.18,30,54 On the other hand, excessive and continuous stress has effects beyond health, triggering diseases, which demonstrates that stress-related events can affect quality of life.55,56
Limitations and Future Directions
An important limitation of this study is its cross-sectional design, which prevents the establishment of a causal relationship between the variables analyzed. Being a cross-sectional study, data were only collected at a specific point in time, which limits the ability to determine the temporal sequence of events or identify the direction of the relationship between variables. Therefore, to establish stronger causal relationships, longitudinal studies are suggested to follow participants over time and assess how changes in the independent variables affect quality of life. Another important limitation of this study is the type of sampling used, which could affect the representativeness of the sample with respect to the target population. In this case, non-probability sampling was used, which implies that the participants were not randomly selected. As a result, the sample may not be fully representative of the target population, limiting the generalizability of the results to other populations or contexts; therefore, it would be advisable to use a probability sample that allows for a random selection of participants. Additionally, it is important to keep in mind that data collected through self-reported online surveys may be subject to possible bias on the part of participants. By relying on self-reporting, there is a possibility that participants may provide incorrect or biased responses due to reasons such as a desire to present themselves in a more favorable light or a lack of accuracy in self-perception. In addition, the absence of direct supervision during data collection may make it difficult to verify the veracity of responses. Therefore, results obtained from self-reported online surveys should be interpreted with caution. Finally, it is important to keep in mind that the largest proportion of the population studied in this study has a fairly young age range, between 20 and 40 years old. Therefore, the associations found in this study may not be generalizable to older adults or to other populations with different demographic characteristics. In fact, the factors that influence quality of life and other variables may vary at different stages of life, and older adults may face different challenges and circumstances that could affect their outcomes.57 In this sense, further research including more representative and diverse samples in terms of age is required to obtain a more complete understanding of the associations between the variables studied.
Practical Implications
Despite these limitations, we believe that our research is valuable, as it is the first to use the EuroQol-5D tool to measure the health status of the Peruvian population. In addition, the results of the study highlight the importance of promoting and encouraging healthy habits, such as a balanced diet, regular physical activity, and proper stress management. These findings support the need to implement health promotion programs that emphasize the adoption of these healthy behaviors in the adult population. This could include promoting activities such as meditation, regular exercise, and seeking social support to reduce stress levels and improve quality of life.
Conclusion
The results of this study demonstrate that different healthy habits can have a positive impact on health-related quality of life in the adult population in Peru. Physical activity, proper sleep habits, and a balanced diet are associated with better health-related quality of life, while drug or tobacco use, and perceived stress are related to a decrease in the same. These results provide public and private healthcare organizations in Peru with the opportunity to develop effective policies to promote healthy habits in the adult population, with the aim of reducing the incidence of non-communicable chronic diseases in the country.
Data Sharing Statement
Data supporting the conclusions of this research will be made available in coordination with the corresponding author.
Funding
Open access funding provided by Universidad Señor de Sipán (DIRECTORY RESOLUTION N 015-2023/ PD-USS) and Universidad Peruana Unión (Grant 041- 2023/SA).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Madeira FB, Filgueira DA, Bosi MLM, et al. Lifestyle, habitus, and health promotion: some approaches. Saude Soc. 2018;27(1):106–115. doi:10.1590/s0104-12902018170520
2. Jacoby E, Goldstein J, López A, et al. Social class, family, and life-style factors associated with overweight and obesity among adults in Peruvian cities. Prev Med. 2003;37(5):396–405. doi:10.1016/S0091-7435(03)00159-2
3. INEI. Peru: Noncommunicable and Communicable Diseases, 2021 – Reports and Publications – National Institute of Statistics and Informatics – Government of Peru, Lima.; 2022. Available from: https://www.gob.pe/institucion/inei/informes-publicaciones/2983123-peru-enfermedades-no-transmisibles-y-transmisibles-2021.
4. Wolniczak I, Cáceres-DelAguila JA, Maguiña JL, et al. Fruits and vegetables consumption and depressive symptoms: a population-based study in Peru. PLoS One. 2017;12(10). doi:10.1371/journal.pone.0186379
5. Paduano D, Cingolani A, Tanda E, et al. Effects of three diets on irritable bowel syndrome and health-related quality of life. Nutrients. 2019;11(7):1566. doi:10.3390/nu11071566
6. Vajdi M, Farhangi MA. A systematic review of the association between dietary patterns and health-related quality of life. Health Qual Life Outcomes. 2020;18(1):1–15. doi:10.1186/s12955-020-01581-z
7. Mantzorou M, Mentzelou M, Vasios GK, et al. Mediterranean diet adherence is associated with favorable health-related quality of life, physical activity, and sleep quality in a community-dwelling Greek older population. Antioxidants. 2023;12(5):983. doi:10.3390/antiox12050983
8. Saintila J, Lozano TE, Ruiz PG, et al. Health-related quality of life, blood pressure, and biochemical and anthropometric profile in vegetarians and nonvegetarians. J Nutr Metab. 2020;2020:1–8. doi:10.1155/2020/3629742
9. Marquez DX, Aguiñaga S, Vásquez PM, et al. A systematic review of physical activity and quality of life and well-being. Transl Behav Med. 2020;10(5):1098–1109. doi:10.1093/tbm/ibz198
10. Snedden TR, Scerpella J, Kliethermes SA, et al. Sport and physical activity level impacts health-related quality of life among collegiate students. Am J Health Promot. 2019;33(5):675–682. doi:10.1177/0890117118817715
11. Ge Y, Xin S, Luan D, et al. Association of physical activity, sedentary time, and sleep duration on the health-related quality of life of college students in Northeast China. Health Qual Life Outcomes. 2019;17(1):1–8. doi:10.1186/s12955-019-1194-x
12. Oh YH, Kim HJ, Kong MH, et al. Association between weekend catch-up sleep and health-related quality of life of Korean adults. Med. 2019;98. doi:10.1097/MD.0000000000014966
13. Barra Almagiá E, Vaccaro Huespe M, de Los A. Perceived stress, coping and hardy personality in infertile women. Liberabit. 2013;19:113–119.
14. Reyna C, Mola DJ, Correa PS. Perceived Stress Scale: psychometric analysis from TCT and IRT. Ansiedad Estrés. 2019;25(2):138–147. doi:10.1016/j.anyes.2019.04.003
15. Parsaei R, Roohafza H, Feizi A, et al. How different stressors affect quality of life: an application of multilevel latent class analysis on a large sample of industrial employees. Risk Manag Healthc Policy. 2020;13:1261–1270. doi:10.2147/RMHP.S256800
16. León-Paucar SD, Calderón-Olivos BC, Calizaya-Milla YE, et al. Depression, dietary intake, and body image during coronavirus disease 2019 quarantine in Peru: an online cross-sectional study. SAGE Open Med. 2021;9:205031212110519. doi:10.1177/20503121211051914
17. Leyton-Román M, Mesquita S, Jiménez-Castuera R. Validation of the Spanish healthy lifestyle questionnaire. Int J Clin Heal Psychol. 2021;21(2):100228. doi:10.1016/j.ijchp.2021.100228
18. Ruisoto P, López-Guerra VM, Paladines MB, et al. Psychometric properties of the three versions of the Perceived Stress Scale in Ecuador. Physiol Behav. 2020;224:113045. doi:10.1016/j.physbeh.2020.113045
19. Herdman M, Badia X, Berra S. EuroQol-5D: a simple alternative for measuring health-related quality of life in primary care. Aten Primaria. 2001;28(6):425–430. doi:10.1016/S0212-6567(01)70406-4
20. Group TE. EuroQol-A new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi:10.1016/0168-8510(90)90421-9
21. Saintila J, Calizaya-Milla YE, Javier-Aliaga DJ. Knowledge of vegetarian and nonvegetarian Peruvian dietitians about vegetarianism at different stages of life. Nutr Metab Insights. 2021;14:117863882199712. doi:10.1177/1178638821997123
22. Ahmad A, Shahril MR, Wan-Arfah N, et al. Changes in health-related lifestyles and food insecurity and its association with quality of life during the COVID-19 lockdown in Malaysia. BMC Public Health. 2022;22(1):1–9. doi:10.1186/s12889-021-12274-7
23. Scala E, Megna M, Amerio P, et al. Patients’ demographic and socioeconomic characteristics influence the therapeutic decision-making process in psoriasis. PLoS One. 2020;15(8):1–14. doi:10.1371/journal.pone.0237267
24. Parmenter BH, Bumrungpert A, Thouas GA. Sociodemographic factors and parental views associated with use of an omega-3 supplement for their children. Pharm Nutr. 2022;20:100289. doi:10.1016/j.phanu.2022.100289
25. Severino R, Espinoza M, Cabieses B. Health-related quality of life by household income in Chile: a concentration index decomposition analysis. Int J Equity Health. 2022;21(1):176. doi:10.1186/s12939-022-01770-w
26. Quarcoopome L, Tornu E. Health-related quality of life of persons living with tuberculosis: a cross-sectional study. J Clin Tuberc Other Mycobact Dis. 2022;28:100324. doi:10.1016/j.jctube.2022.100324
27. Hidalgo-rasmussen CA Actividad física, conductas sedentarias y calidad de vida en adolescentes universitarios de Ciudad Guzmán, Jalisco, México [Physical activity, sedentary behavior and quality of life in undergraduate adolescents of Ciudad Guzman, State of Jalisco, Mex]; 1943:1943–1952. Spanish.
28. Antunes R, Fonseca E. Qualidade de vida, vitalidade e força de preensão manual em idosos praticantes de exercício físico [Quality of life, vitality and handgrip strength in elderly practitioners of physical exercise]; 2022:245–255. Spanish.
29. Zurita-Ortega F, Salvador-Pérez F, Knox E, et al. Actividad física y calidad de vida relacionada con la salud en esco-lares: análisis mediante ecuaciones estructurales [Physical activity and health-related quality of life in schoolchildren: structural equations analysis]. An Psicol. 2018;34(2):385–390. Spanish. doi:10.6018/analesps.34.2.299781
30. Qi M, Li P, Moyle W, et al. Physical activity, health-related quality of life, and stress among the Chinese adult population during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(18):1–10. doi:10.3390/ijerph17186494
31. Amit Aharon A, Dubovi I, Ruban A. Differences in mental health and health-related quality of life between the Israeli and Italian population during a COVID-19 quarantine. Qual Life Res. 2021;30(6):1675–1684. doi:10.1007/s11136-020-02746-5
32. Davila-Torres DM, Vilcas-Solís GE, Rodríguez-Vásquez M, et al. Eating habits and mental health among rugby players of the Peruvian pre-selection during the second quarantine due to the COVID-19 pandemic. SAGE Open Med. 2021;9:205031212110437. doi:10.1177/20503121211043718
33. Fuenzalida CD, Morales AM, Campos HR, et al. Relationship between physical activity and quality of life in youth during the COVID-19 pandemic. Rev Cuba Med Mil. 2021;50(4). https://www.scopus.com/record/display.uri?eid=2-s2.0-85119494569&origin=resultslist&sort=plf-f&src=s&sid=0e2c078daf591d090b3f62679b968b49&sot=b&sdt=b&s=TITLE-ABS-KEY%28Relationship+between+physical+activity+and+quality+of+life+in+youth+during+the+COVID-19+pandemic%29&sl=111&sessionSearchId=0e2c078daf591d090b3f62679b968b49
34. Huancahuire-Vega S, Newball-Noriega EE, Rojas-Humpire R, et al. Changes in eating habits and lifestyles in a Peruvian population during social isolation for the COVID-19 pandemic. J Nutr Metab. 2021;2021:1–11. doi:10.1155/2021/4119620
35. Poudel AN, Zhu S, Cooper N, et al. Impact of Covid-19 on health-related quality of life of patients: a structured review. PLoS One. 2021;16(10). doi:10.1371/JOURNAL.PONE.0259164
36. Ahn SN. The potential impact of COVID-19 on health-related quality of life in children and adolescents: a systematic review. Int J Environ Res Public Health. 2022;19:14740. doi:10.3390/ijerph192214740
37. Milic M, Gazibara T, Pekmezovic T, et al. Tobacco smoking and health-related quality of life among university students: mediating effect of depression. PLoS One. 2020;15(1):1–18. doi:10.1371/journal.pone.0227042
38. Sagtani RA, Thapa S, Sagtani A. Smoking, general and oral health related quality of life – A comparative study from Nepal. Health Qual Life Outcomes. 2020;18(1):1–7. doi:10.1186/s12955-020-01512-y
39. Marquez-Arrico JE, Navarro JF, Adan A. Health-related quality of life in male patients under treatment for substance use disorders with and without major depressive disorder: influence in clinical course at one-year follow-up. J Clin Med. 2020;9(10):1–19. doi:10.3390/jcm9103110
40. Canto EG, Guillamon AR, López LN. Nivel de actividad física, consumo habitual de tabaco y alcohol, y su relación con la calidad de vida en adolescentes españoles [Physical activity level, tobacco and alcohol habitual consumption, and its relationship with quality of life in Spanish adol]. Retos. 2021;39:112–119. Spanish.
41. Latorre-Román PÁ, Gallego-Rodríguez M, Mejía-Meza JA, et al. Tobacco and alcohol consumption and sports practice in Mexican and Spanish university students: association with health-related quality of life and sensation seeking. Gac Med Mex. 2015;151(2):197–205.
42. Kesztyüs D, Fuchs M, Cermak P, et al. Associations of time-restricted eating with health-related quality of life and sleep in adults: a secondary analysis of two pre-post pilot studies. BMC Nutr. 2020;6(1):4–11. doi:10.1186/s40795-020-00402-2
43. Dai H, Mei Z, An A, et al. Association between sleep problems and health-related quality of life in Canadian adults with chronic diseases. Sleep Med. 2019;61:26–30. doi:10.1016/j.sleep.2019.04.015
44. Leng M, Yin H, Zhang P, et al. Sleep quality and health-related quality of life in older people with subjective cognitive decline, mild cognitive impairment, and Alzheimer disease. J Nerv Ment Dis. 2020;208(5):387–396. doi:10.1097/NMD.0000000000001137
45. Baek Y, Jung K, Kim H, et al. Association between fatigue, pain, digestive problems, and sleep disturbances and individuals’ health-related quality of life: a nationwide survey in South Korea. Health Qual Life Outcomes. 2020;18(1):1–9. doi:10.1186/s12955-020-01408-x
46. Zou S, Feng G, Li D, et al. Lifestyles and health-related quality of life in Chinese people: a national family study. BMC Public Health. 2022;22(1):1–10. doi:10.1186/s12889-022-14680-x
47. Banda-Ccana DE, Infantes-Ruiz VH, Calizaya-Milla YE, et al. Dieta y riesgo de enfermedades mentales en adultos peruanos, estudio transversal [Diet and risk of mental illness in Peruvian adults, cross-sectional study]. Arch Latinoam Nutr. 2021;71(3):199–207. Spanish. doi:10.37527/2021.71.3.004
48. Nuñez-Leyva RE, Lozano-López TE, Calizaya-Milla YE, et al. Excess weight and body fat percentage associated with waist circumference as a cardiometabolic risk factor in university students. Scientifica. 2022;2022:1–8. doi:10.1155/2022/1310030
49. Knox E, Muros JJ. Association of lifestyle behaviours with self-esteem through health-related quality of life in Spanish adolescents. Eur J Pediatr. 2017;176(5):621–628. doi:10.1007/s00431-017-2886-z
50. Yan LL, Li C, Zou S, et al. Healthy eating and all-cause mortality among Chinese aged 80 years or older. Int J Behav Nutr Phys Act. 2022;19(1):1–12. doi:10.1186/s12966-022-01280-6
51. Bytyci-Katanolli A, Merten S, Kwiatkowski M, et al. Non-communicable disease prevention in Kosovo: quantitative and qualitative assessment of uptake and barriers of an intervention for healthier lifestyles in primary healthcare. BMC Health Serv Res. 2022;22(1):1–17. doi:10.1186/s12913-022-07969-5
52. Hart LM, Gordon AR, Sarda V, et al. The association of disordered eating with health-related quality of life in U.S. young adults and effect modification by gender. Qual Life Res. 2020;29(5):1203–1215. doi:10.1007/s11136-019-02396-2
53. Xiao Y, Wang H, Zhang T, et al. Psychosocial predictors of physical activity and health-related quality of life among Shanghai working adults. Health Qual Life Outcomes. 2019;17(1):1–9. doi:10.1186/s12955-019-1145-6
54. Guerra F, Corridore D, Peruzzo M, et al. Quality of life and stress management in healthcare professionals of a dental care setting at a teaching hospital in Rome: results of a randomized controlled clinical trial. Int J Environ Res Public Health. 2022;19(21):13788. doi:10.3390/ijerph192113788
55. Ribeiro ÍJS, Pereira R, Freire IV, et al. Stress and quality of life among university students: a systematic literature review. Heal Prof Educ. 2018;4:70–77.
56. Alkatheri AM, Bustami RT, Albekairy AM, et al. Quality of life and stress level among health professions students. Heal Prof Educ. 2020;6:201–210.
57. Frías-Luque MD, Toledano-González A. Determinants of quality of life and well-being in cognitively unimpaired older adults: a systematic review. PeerJ. 2022;10:e12900. doi:10.7717/peerj.12900