Car-centric lifestyle and an epidemic of loneliness are among reasons American life expectancy is falling behind its peers
Despite the glitz, glamour and claims of being the ‘greatest country in the world’, Americans are falling behind their peers in one crucial area.
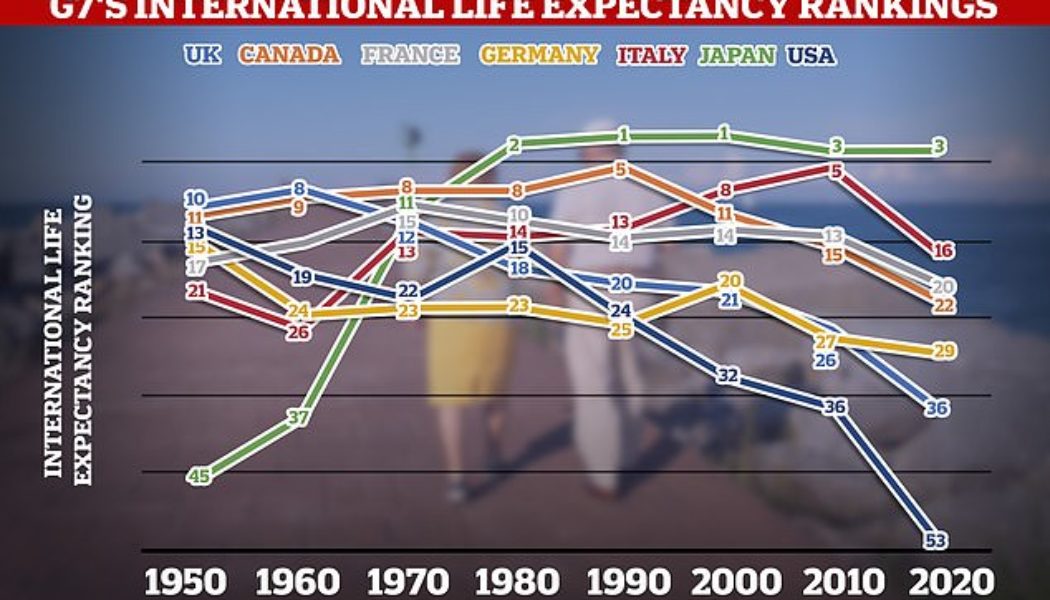
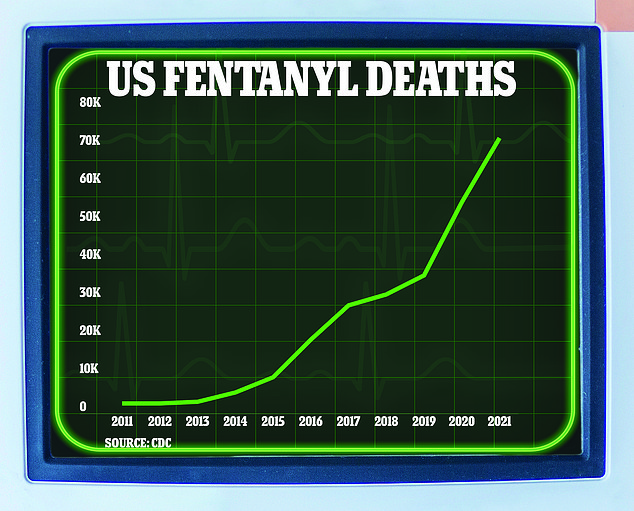
Life expectancy in the US falls well below many of its peer nations. A British analysis of international data published this week found it has the worst standing of any G7 nation.
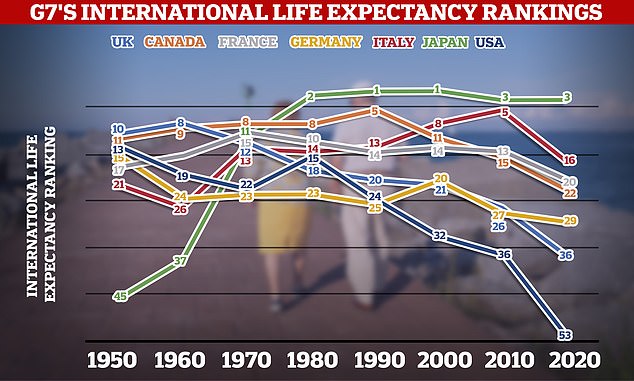
At 79 years, the US life expectancy falls three years short of its northern neighbor, Canada, and behind virtually every western European nation. Americans live the 53rd longest lives — far from the heights many would expect.
This comes despite Americans spending more on health care than their peer nations, according to a Commonwealth Fund study earlier this year.
While many factors play a role, the car-centric culture, poor food choices and price of health care, among other reasons, are at the heart of why the US is lagging behind.
The alarming study published last week by Oxford University and the London School of Hygiene and Tropical Medicine shines a spotlight on America’s failings.
It paid a particular focus on G7 nations, which combine represent around half of the global economy. They include the US, UK, Canada, France, Germany, Italy and Japan.
While global lifespans have greatly increased across the world in recent years, America has fallen off the pace of its peers.
Ranking 13th in the world in the US, the nation has plummeted out of the top rungs in recent decades. Between 2010 and 2020, America fell from 36th to the 50s.
This is despite America’s large spending on health care. The Commonwealth Fund report found that the US spends 17.8 percent of its GDP on health costs.
No other developed nation included in the global study surpassed 13 percent, and the UK fell at just under 12 percent.
So, despite this spending, why has America fallen so far behind?
Car centric lifestyle leaves Americans sedentary, pollutes the air
Many Americans rarely walk anywhere. An estimated 76 percent of the population drives to and from work each day, with only three percent walking.
In many parts of the US, walking to-and-from locations is almost unfeasible. Studies cite New York City, San Francisco, Boston and Baltimore as the US’ most walkable places, but only five percent of the nation’s population occupies those areas.
This leads to many Americans not getting nearly enough physical activity each day.
Experts recommend a person takes 10,000 steps daily. A 2010 study from the University of Colorado, Denver found that people in the US only get around 5,000 on average.
This falls well short of other nations included in the study, such as Japan (7,168 daily steps on average), Switzerland (9,650) and West Australia (9,695).
Not getting enough daily activity can lead to heart disease, obesity, diabetes, high blood pressure and other conditions that harm heart, and overall body health.
Sitting for long periods of time each day — which many Americans do between their car, desk at work and the couch at home — can open a wealth of issues.
The Mayo Clinic warns sitting for an extended period each day can cause many of the same issues and lead to the development of dangerous visceral fat in the midsection.
A car-centric lifestyle also requires roads to be built everywhere — including near American homes.
Cars emit dangerous gasses such as carbon monoxide and types of nitrogen oxide.
Constantly being exposed to these gasses can increase a person’s likelihood of suffering potentially devastating diseases — especially for children.
Studies have linked living near a highway or major road to increased rates of asthma, chronic obstructive pulmonary disease and diabetes.
Guns and drugs
Gun violence has reached an epidemic point in the US.
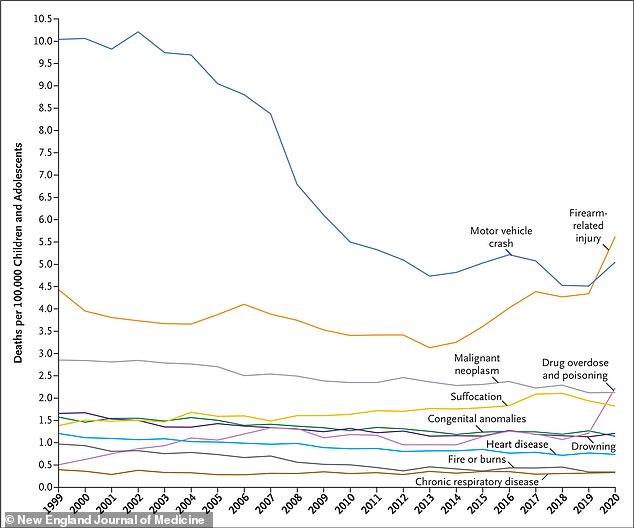
Firearms have surpassed car crashes and all other injuries as the leading cause of death for American children. The rate of gun deaths in children is nearing five for every 100,000.
Events of mass violence caused by guns occur alarmingly often in the US. 2021 saw 690 mass shooting events, defined as situations in which at least four people are shot and either injured or killed, not including the shooter. In 2021, that tally hit 647.
The majority of deaths caused by guns, however, are suicides. Data for 2022 on suicide deaths caused by guns is still pending, but in 2021 that figure was 26,328.
The immense toll that guns have had on Americans’ overall health is staggering and unrivaled by any other country.
Firearms have cost Americans millions of years of potential life – 12.6million years between 2009 and 2018 to be exact, according to a 2022 analysis published in the journal Trauma Surgery & Acute Care Open.
The researchers behind the study, led by Dr Joshua Klein at Westchester Medical Center in New York, calculated lives lost based on an average life expectancy of 80 years old – slightly higher than the 2020 average of 77 years.
White males, who accounted for the majority of gun deaths, lost the most potential years of life due to suicide by gun, with 4.95 million potential years lost during the 10-year study period.
Homicide by firearm constituted about 1.7 million years lost.
While women were less likely to die by firearm, suicides by guns are on the rise. Women lost more than 867,000 years of potential life due to suicide.
A team of researchers at Boston University, meanwhile, reported that from 2000 to 2016, guns led to an overall drop in Americans’ life expectancy by nearly two and a half years.
It’s no secret that the Covid-19 pandemic has devastated millions of families across the US.
In 2021, life expectancy fell in the US for the second year in a row, from 79 in 2019 to 77 in 2020 and finally to 76.1 a year later.
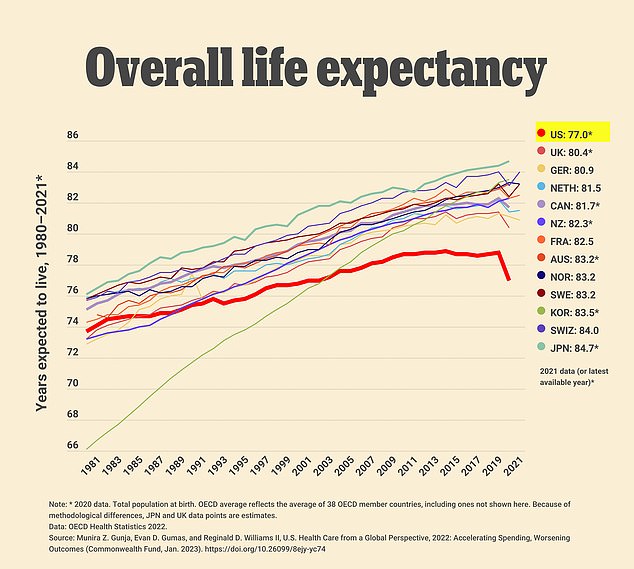
But life expectancy had been on the decline even before due to Americans’ penchant for alcohol and drugs.
Substance abuse deaths have contributed to an overall rise in so-called ‘deaths of despair’ fueled by drugs, alcohol, and suicides.
Drug overdoses have led to almost a million deaths since 1999 and nearly 650,000 of those deaths were caused by opioids.
Nearly 107,000 Americans died of an opioid overdose in 2021, the highest on record, about double the total recorded in 2015.
This astronomical level of preventable mortality is a sharp contrast to peer nations.
US drug overdose deaths are much higher than in other high-income countries. An analysis by the Commonwealth Fund estimated drug overdoses to have cost 320 lives per million residents in 2021.
Scotland, which has long reported higher overdose mortality than the rest of the UK, follows the US at 267 deaths per million residents. Then comes Canada with an opioid-related death rate of 171 deaths per million residents.
And all other countries in the report by Commonwealth are below 100 deaths per million residents.
American food — highly processed, filled with calories, sugar and fats
The average American’s diet is devastatingly unhealthy.
Highly processed foods — which are so bad that some scientists believe they should be classified as drugs — raise risks of cancers and Alzheimer’s in frequent eaters.
‘They are industrially produced substances designed to deliver sugar and fat,’ Dr Alexandra DiFeliceantonio, a health behaviors research professor at Virginia Tech University, told DailyMail.com in February.
‘They are not foods anymore. These are these products that have been really well designed to deliver addictive substances.’
In February, a British study found people who regularly indulged in these foods were 30 percent more likely to die from cancer. Breast and ovarian cancer were specifically highlighted, with women suffering a larger risk.
This is because of the many chemicals used in them for flavoring, preservation, texture and color.
These foods also come with high calorie and sodium counts, building the likelihood a person suffers from obesity, high blood pressure and other related heart issues.
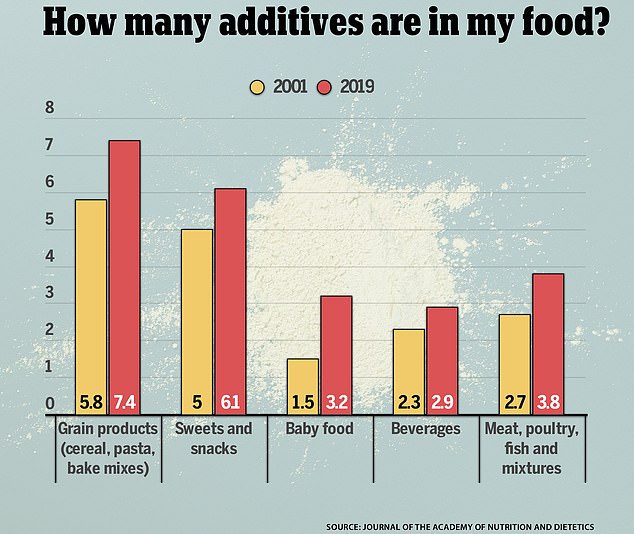
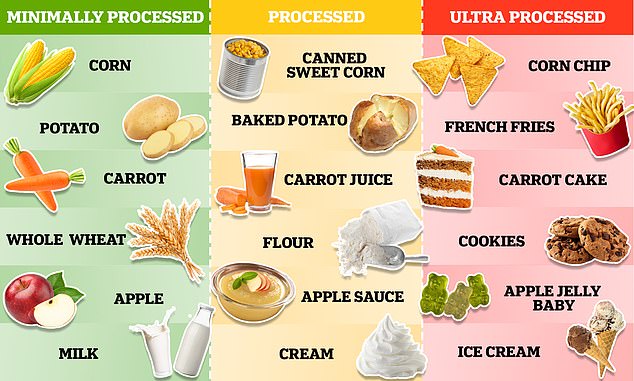
Processed foods are, unfortunately, a significant part of the average American’s diet.
A University of North Carolina study published earlier this month found that 60 percent of food consumed in the US contains these harmful additives.
In February, the University of Michigan researchers found that 13 percent of people 50 or older were addicted to these foods.
These foods have been mainly responsible for America’s crisis with weight and diabetes.
The Centers for Disease Control and Prevention (CDC) estimates that 42 percent of Americans are obese. This is included in the 70 percent that are overweight.
Around 10 percent, or nearly 30million, Americans suffer from the potentially devastating metabolic disease diabetes.
For comparison, 25 percent of Britons are obese and just under 40 percent of overweight. While these levels have sparked panic across the pond, they fall well below the US’ numbers.
Health care is both expensive and far
The US far outspends peer countries such as the UK, Germany, Sweden, and Japan on healthcare, yet Americans have the lowest life expectancy among them.
Unlike most of these comparable countries, the US government does not guarantee government, or public, health coverage to all their residents.
In fact, the US is the only high-income country where a substantial portion of the population – about 30 million Americans – lacks any form of health insurance.
This means that unless covered by a federal program such as Medicare, which services seniors, or Medicaid, which covers the very poor, or by a private health insurance plan that requires paying a monthly premium and deductable, millions of Americans pay for healthcare services out of pocket, which can be astronomical.
In the US, the private market dominates the healthcare sector. Hospital services cost more, drugs, especially newly-developed ones, are more expensive, and doctors fetch higher salaries.
A general physician in America makes an average salary of about $218,000 per year, compared to their counterparts in 10 other high-income countries where the salary range was $86,600 to about $154,000.
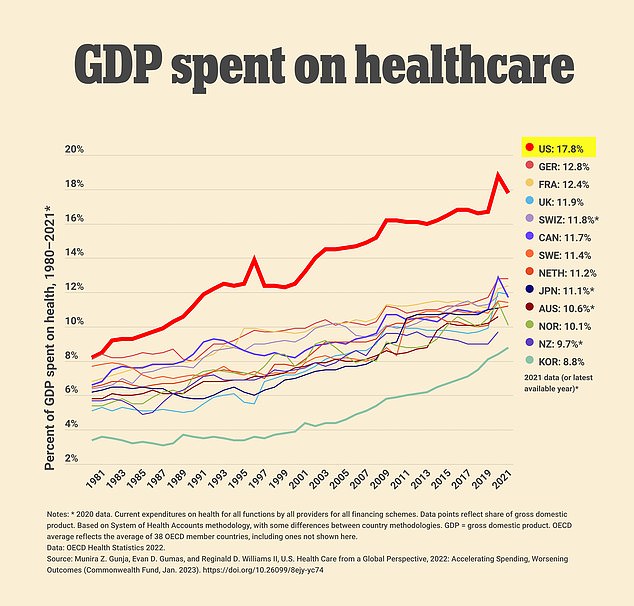
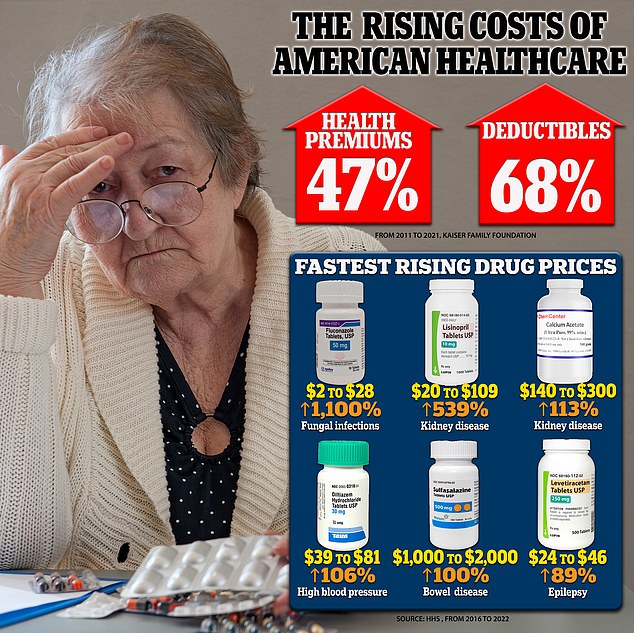
Further, per capita spending for pharmaceuticals in the US was more than $1,400 compared with a range of $466 to $939 in other nations.
Individual services themselves are more expensive in the US compared to other countries. Harvard University researchers reported that in 2013, the average cost in the US was $75,345 for a coronary artery bypass graft surgery, whereas the costs in the Netherlands and Switzerland were $15,742 and $36,509, respectively.
Exorbitant costs of care in the US leads many Americans to put off preventative services and seeking care when they need it.
A recent Gallup poll found that 38 percent of Americans are putting off medical treatment because of financial concerns – the highest ever recorded and up 12 percent from last year.
Something as simple as distance to a hospital can have a major impact on an entire region’s overall health. In general, rural populations have poorer health outcomes than surban and urban ones due to a variety of factors ranging from less health insurance coverage to inaccessibility to care.
Rural Americans live an average of 10.5 miles from the nearest hospital, compared with 5.6 miles for people in suburban areas and 4.4 for those in urban areas, according to a Pew Research Center analysis.
A nationally representative study in 2018 reported that over 11 percent of respondents who live outside a metropolitan area reported their health status as ‘fair’ or ‘poor’ compared to about eight percent of respondents from large metropolitan centers.
Americans and lonely
Loneliness and social isolation are significant risk factors for early death in the US.
Former United States Surgeon General Vivek Murthy even named loneliness a public health crisis.
Dr Murthy said: ‘In the long term, the stress state triggered by chronic loneliness can increase levels of inflammation in our body and increase our risk for illness.’
‘This likely explains why loneliness is associated with higher risk of heart disease, dementia, depression, and anxiety. When we’re chronically lonely, it also affects how we show up at work and for our families.’
Isolation and loneliness are associated with about a 30 percent increased risk of heart attack or stroke, or death from either, according to the American Heart Association.
Human beings are an intrinsically community-oriented species. We were built to thrive in groups.
Yet, despite an increasingly connected world thanks to innovations in technology, Americans are lonlier than ever before.
A Harvard survey of American adults found that 36 percent of respondents reported serious loneliness—feeling lonely ‘frequently’ or ‘almost all the time or all the time’ in the four weeks prior to the survey.
This included 61 percent of young people aged 18 to 25 and 51 percent of mothers with young children.
The pervasive sense of loneliness has only driven up rates of premature death. Meta-analyses from Brigham Young University in Utah found that the risk of early death associated with loneliness, social isolation, and living alone was equal to or greater than the premature death risk associated with obesity and other major health conditions.

Feeling lonely, unhappy and hopeless has also been found to add up to an extra year and eight months onto someone’s age — five months more than smoking.
Experts believe chronic inflammation caused by being unhappy causes damage to cells and vital organs.
Loneliness also has a major bearing on mental wellbeing. The number of Americans committing suicide is almost back at record levels after the Covid pandemic, according to official figures.
There were 48,183 suicides in 2021, according to the Centers for Disease Control and Prevention (CDC), which was just 161 deaths below the record in 2018. That is the equivalent of a suicide every 10 minutes throughout the whole of 2021.
The risk of death due to loneliness tends to increase with age, as more people are prone to experience widowhood, retirement, and other life-changing events.
Nearly one-quarter of U.S. adults ages 65 and older are socially isolated, and prevalence of loneliness is even higher, with estimates ranging from 22 to 47 percent.
The high rates of loneliness and isolation increased still further during the Covid-19 pandemic, especially among young adults 18 to 25, seniors, and the poor.